GERD
Gastroesophageal reflux disease (GERD) is a condition in which your stomach contents and gastric acid back up into your esophagus, causing a burning sensation in your throat and chest. GERD happens when a muscle located at the end of your esophagus does not function properly and allows leakage. It affects about 40 million people in the United States.
At St. Elizabeth Healthcare we are dedicated to helping you achieve the highest level of health possible. Our multidisciplinary care team works with you to determine what is affecting your health and what we can do to help you feel better.
Symptoms of GERD
The most common symptom of GERD is heartburn – a painful, burning sensation in the middle of your chest, behind your breastbone and the upper part of your abdomen.
Other symptoms may include:
- Regurgitation
- Chest pain
- Difficulty swallowing
- Nausea and vomiting
- Difficulty breathing
- Voice hoarseness
- Cough

Learn More
For more information or to schedule an appointment with the St. Elizabeth Thoracic Surgery office, call
(859) 301-2465.
Causes of GERD
GERD occurs when the sphincter muscle in your lower esophagus becomes weak. As a result, your stomach contents and gastric acid can back up into your esophagus, causing GERD. This can be caused by a hiatal hernia but not all patients with GERD will have a hiatal hernia.
Diagnosing GERD
Tests and procedures that may be used to diagnose GERD include:
- Barium swallow – X-rays of your digestive tract are taken after you drink a solution containing barium.
- Upper endoscopy (EGD) – a test to examine the lining of your esophagus, stomach and the first part of your small intestine.
- Esophageal manometry – a test to measure the muscle contractions of your esophagus.
- pH monitoring/testing
Treating GERD
Most cases of GERD can be treated effectively with medication and lifestyle changes. The goal of drug therapy is to reduce the level of acid in your stomach to relieve the symptoms of heartburn. Lifestyle changes like quitting smoking, weight loss and avoiding foods that cause symptoms may also offer relief of GERD symptoms.
About 20-30% of patients will still have persistent symptoms despite medical management or may require escalating doses of acid medications. In these cases, surgery may be considered. The thoracic surgeons at St. Elizabeth Healthcare are dedicated exclusively to surgery to treat diseases of the esophagus and lung. They have a level of expertise and training not available anywhere else in this region so you can rest assured you are receiving the best care possible.
Surgical Treatment Options:
Laparoscopic surgery with Nissen fundoplication
Laparoscopic surgery with Nissen fundoplication is the conventional surgery used to treat GERD. During laparoscopic surgery, several small incisions are made in your abdomen.
These are used to insert surgical instruments and a laparoscope – a small thin tube with a video camera attached that allows your surgeon to see inside your body during surgery.
If a hernia is present, the stomach is moved into its proper position and the opening allowing it to move out of place is closed.
Fundoplication is a way to restore the function of your lower esophagus by wrapping it with the upper part of your stomach. The process creates a new valve between your esophagus and your stomach and prevents the contents from your stomach from backing up into your esophagus.
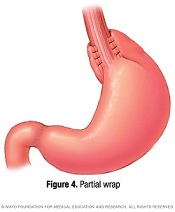
Partial Fundoplication
Some patients may not have an adequate esophageal squeeze for a Nissen Fundoplication so a partial fundoplication may be considered for these situations. In a partial fundoplication, the upper part of the stomach is only partially wrapped around the lower esophagus.
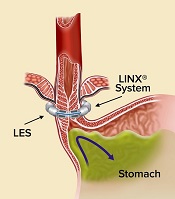
Magnetic Sphincter Augmentation – LINX Procedure
LINX is an alternative and minimally invasive surgical procedure for people with GERD.
It uses a small, flexible band of titanium magnetic beads to help the valve muscle in your esophagus stay closed when it should. When you swallow, the beads separate to allow your food and/or liquid to move into your stomach. However, after the meal the stomach cannot generate enough force to separate the beads to allow reflux. As compared to fundoplication, LINX works like more of a two-way valve allowing you to burp and blech normally preventing side effects such as gas/bloating symptoms which can be experienced with Nissen fundoplication. However, LINX does not alter your stomach and normal anatomy is preserved.
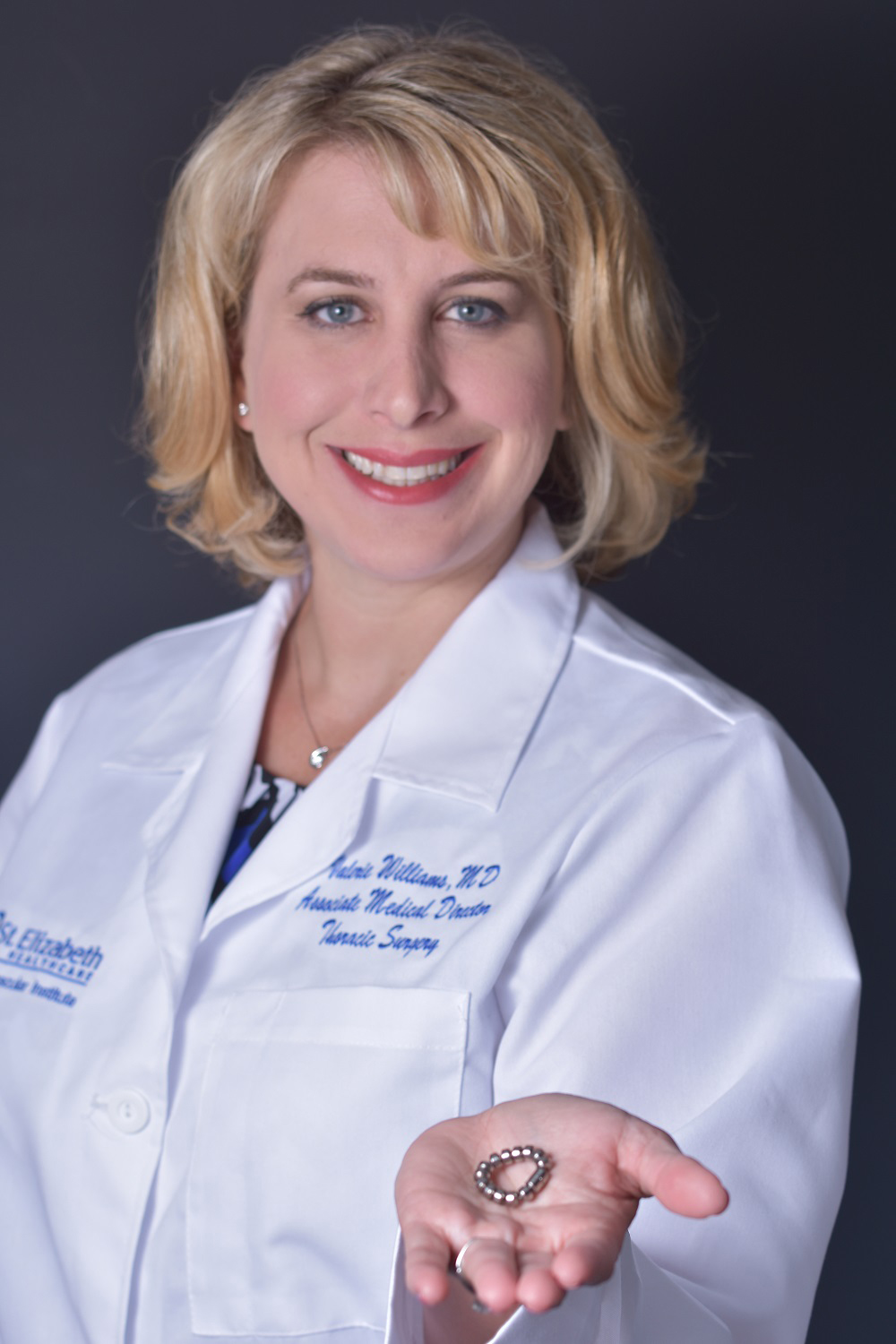
Dr. Valerie Williams at St. Elizabeth Healthcare is the only surgeon in this area to offer LINX.
LINX is a revolutionary solution for GERD proven to eliminate dependence on medication and improve quality of life. LINX is constructed of titanium and with permanent magnets.
5-year results of a landmark study confirm the LINX procedure as a beneficial treatment for GERD.
- 85% of patients remained free from dependence on daily GERD medication.
- Bothersome regurgitation, was eliminated in 99% of patients.
- Bothersome heartburn, was significantly reduced from 89% at baseline to 11.9%.
- Patients reported a significant improvement in their quality of life.
Surgical Treatment for GERD After Weight Loss Surgery
Treatment options for GERD after sleeve gastrectomy have been limited. Some patients with severe and persistent symptoms often would be offered a conversion of their sleeve to a gastric bypass, which is a more invasive surgery and is not appropriate for those who are back to their normal weight.
Magnetic Sphincter Augmentation (MSA) LINX™ Procedure – Post-Sleeve Procedure
 The MSA procedure is approved for post-sleeve patients and has shown positive results in treating GERD and has proven to be highly effective. GERD occurs because the valve at the bottom of the esophagus is weak or defective. The MSA procedure uses a flexible chain of small titanium beads that have magnetic cores, much like a bracelet. It is placed around the lower esophagus to recreate a barrier to prevent harmful stomach acids from entering the esophagus.
The MSA procedure is approved for post-sleeve patients and has shown positive results in treating GERD and has proven to be highly effective. GERD occurs because the valve at the bottom of the esophagus is weak or defective. The MSA procedure uses a flexible chain of small titanium beads that have magnetic cores, much like a bracelet. It is placed around the lower esophagus to recreate a barrier to prevent harmful stomach acids from entering the esophagus.
Some weight loss surgery patients may have had GERD before their surgery. Others can develop GERD symptoms after their weight loss surgery. In patients who have persistent symptoms of GERD after sleeve gastrectomy, recent studies show that with MSA, 85% of patients are off a daily PPIs (Proton Pump Inhibitors) at one year and 92% are free of moderate to severe regurgitation (occurs when stomach contents move upwards into the esophagus) one year after the procedure.
Not everyone who has had a sleeve gastrectomy is a candidate for the MSA procedure, but surgeons look at those patients who meet the following criteria:
- Body Mass Index (BMI) of less than 35.
- Are at least one year out from weight loss surgery.
Surgeons also conduct a full evaluation and determine if the patient has a normal squeeze of the esophagus (from top to bottom) and if the anatomy of the remaining stomach is appropriate.
Chelsie Begley
Gastroesophageal reflux disease (GERD) affects more than 20% of Americans. GERD causes heartburn, chest pain, inability to eat certain foods and even food regurgitation – symptoms that were a big part of 27-year-old Chelsie Begley’s daily life.
Schedule an Appointment Today
Call Us to Schedule a Visit
For more information or to schedule an appointment with the St. Elizabeth Thoracic Surgery office, please call
(859) 301-2465.