Frozen shoulder
Updated: 2022-08-19
Overview
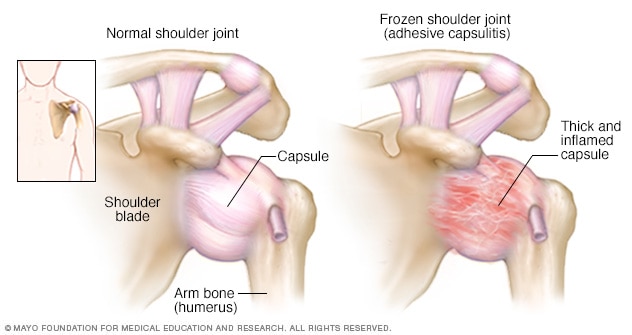
Frozen shoulder
Frozen shoulder occurs when the connective tissue enclosing the joint thickens and tightens.
Frozen shoulder, also called adhesive capsulitis, involves stiffness and pain in the shoulder joint. Signs and symptoms typically begin slowly, then get worse. Over time, symptoms get better, usually within 1 to 3 years.
Having to keep a shoulder still for a long period increases the risk of developing frozen shoulder. This might happen after having surgery or breaking an arm.
Treatment for frozen shoulder involves range-of-motion exercises. Sometimes treatment involves corticosteroids and numbing medications injected into the joint. Rarely, arthroscopic surgery is needed to loosen the joint capsule so that it can move more freely.
It's unusual for frozen shoulder to recur in the same shoulder. But some people can develop it in the other shoulder, usually within five years.
Symptoms
Frozen shoulder typically develops slowly in three stages.
- Freezing stage. Any movement of the shoulder causes pain, and the shoulder's ability to move becomes limited. This stage lasts from 2 to 9 months.
- Frozen stage. Pain might lessen during this stage. However, the shoulder becomes stiffer. Using it becomes more difficult. This stage lasts from 4 to 12 months.
- Thawing stage. The shoulder's ability to move begins to improve. This stage lasts from 5 to 24 months.
For some people, the pain worsens at night, sometimes disrupting sleep.
Causes
The shoulder joint is enclosed in a capsule of connective tissue. Frozen shoulder occurs when this capsule thickens and tightens around the shoulder joint, restricting its movement.
It's unclear why this happens to some people. But it's more likely to happen after keeping a shoulder still for a long period, such as after surgery or an arm fracture.
Risk factors
Certain factors may increase the risk of developing frozen shoulder.
Age and sex
People 40 and older, particularly women, are more likely to have frozen shoulder.
Immobility or reduced mobility
People who've had to keep a shoulder somewhat still are at higher risk of developing frozen shoulder. Restricted movement can be the result of many factors, including:
- Rotator cuff injury
- Broken arm
- Stroke
- Recovery from surgery
Systemic diseases
People who have certain diseases appear more likely to develop frozen shoulder. Diseases that might increase risk include:
- Diabetes
- Overactive thyroid (hyperthyroidism)
- Underactive thyroid (hypothyroidism)
- Cardiovascular disease
- Parkinson's disease
Prevention
One of the most common causes of frozen shoulder is not moving a shoulder while recovering from a shoulder injury, broken arm or stroke. If you've had an injury that makes it difficult to move your shoulder, talk to your health care provider about exercises that can help you maintain your ability to move your shoulder joint.
Diagnosis
During the physical exam, a health care provider might ask you to move your arm in certain ways. This is to check for pain and see how far you can move your arm (active range of motion). Then you might be asked to relax your muscles while the provider moves your arm (passive range of motion). Frozen shoulder affects both active and passive range of motion.
Frozen shoulder can usually be diagnosed from signs and symptoms alone. But imaging tests — such as X-rays, ultrasound or MRI — can rule out other problems.
Treatment
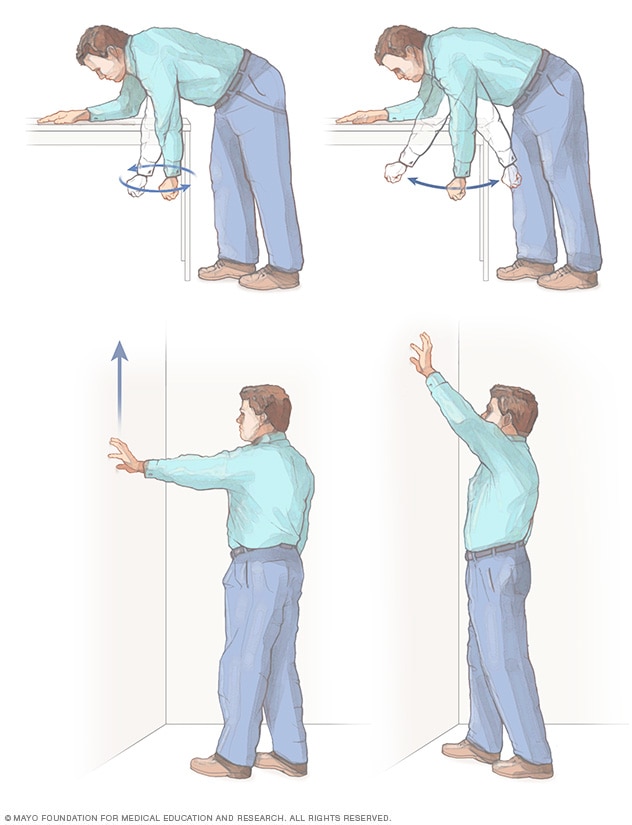
Shoulder exercises
These exercises may improve your shoulder's range of motion. Let your arm hang down like a pendulum, and then gently swing it back and forth or in circles. Pretend your fingers are your feet and walk your fingers up a wall.
Most frozen shoulder treatment involves controlling shoulder pain and preserving as much range of motion in the shoulder as possible.
Medications
Pain relievers such as aspirin and ibuprofen (Advil, Motrin IB, others) can help reduce pain and inflammation associated with frozen shoulder. In some cases, a health care provider might prescribe stronger pain-relieving and anti-inflammatory drugs.
Therapy
A physical therapist can teach you range-of-motion exercises to help recover your shoulder movement. Your commitment to doing these exercises is necessary to regain as much movement as possible.
Surgical and other procedures
Most frozen shoulders get better on their own within 12 to 18 months. For severe or persistent symptoms, other treatments include:
- Steroid injections. Injecting corticosteroids into the shoulder joint might help decrease pain and improve shoulder mobility, especially if given soon after frozen shoulder begins.
- Hydrodilatation. Injecting sterile water into the joint capsule can help stretch the tissue and make it easier to move the joint. This is sometimes combined with a steroid injection.
- Shoulder manipulation. This procedure involves a medication called a general anesthetic, so you'll be unconscious and feel no pain. Then the care provider moves the shoulder joint in different directions to help loosen the tightened tissue.
- Surgery. Surgery for frozen shoulder is rare. But if nothing else helps, surgery can remove scar tissue from inside the shoulder joint. This surgery usually involves making small incisions for small instruments guided by a tiny camera inside the joint (arthroscopy).
Lifestyle and home remedies
Continue to use the shoulder and arm as much as possible given your pain and range-of-motion limits. Applying heat or cold to your shoulder can help relieve pain.
Alternative medicine
Acupuncture
Acupuncture uses hair-thin, flexible needles put into the skin at certain points on the body. Typically, the needles remain in place for 15 to 40 minutes. The needles are not generally put in very far. Most acupuncture treatments are relatively painless.
Nerve stimulation
A transcutaneous electrical nerve stimulation (TENS) unit delivers a tiny electrical current to key points on a path that a nerve follows. The current, delivered through electrodes taped to the skin, isn't painful or harmful. It's not known exactly how TENS works. It might cause the release of molecules that curb pain (endorphins) or block fibers that carry pain.
Preparing for an appointment
You might first see your primary care provider. In some cases, you may be referred to a doctor who specializes in treating bones and muscles (orthopedist or physiatrist).
What you can do
Before your appointment, be prepared with:
- A complete description of your symptoms and when they began
- Information about medical problems you've had
- Information about the medical problems of your parents or siblings
- The names of all the medications and dietary supplements you take
- Questions to ask the health care provider
What to expect from your doctor
Be prepared to answer questions, such as:
- What worsens your symptoms?
- Have you ever injured that shoulder? If so, how?
- Do you have diabetes?
- Have you had recent surgeries or had to keep your shoulder still for a time?