Blood sugar testing: Why, when and how
Blood sugar testing is an important part of diabetes care. Find out when to test your blood sugar, how to use a blood sugar meter and more.
Updated: 2024-01-16
If you have diabetes, testing your blood sugar levels can be a key part of staying healthy. Blood sugar testing helps many people with diabetes manage the condition and prevent health problems.
There are several main ways to test your blood sugar. You can use a device that measures your sugar levels throughout the day and night with a tiny sensor. This is called a continuous glucose monitor (CGM). Or you can test yourself as needed with a portable electronic device that uses a small drop of blood. This is called a blood sugar meter.
Why test blood sugar
Blood sugar testing gives useful information to manage diabetes. It can help you:
- Track the effect of diabetes medicine on blood sugar levels.
- Adjust doses of diabetes medicines with the guidance of your treatment team.
- Find out if blood sugar levels are high or low. Then, if needed, change treatment to treat high blood sugar or take fast-acting carbohydrates to treat low blood sugar.
- Track progress in reaching your treatment goals.
- Learn how diet and exercise affect blood sugar levels.
- Understand how other factors, such as sickness or stress, affect blood sugar levels.
When to test blood sugar
Your healthcare professional can tell you how often to check your blood sugar levels. Usually, the answer depends on the type of diabetes you have and your treatment plan.
Type 1 diabetes
Your healthcare professional may suggest a CGM or blood sugar testing 4 to 10 times a day if you have type 1 diabetes. You may need to test:
- Before meals and snacks, and sometimes after meals.
- Before, after and sometimes during exercise.
- Before bed.
- Sometimes, during the night.
- After treating low blood sugar.
- More often if you're sick.
- More often if you change your daily routine.
- More often if you start a new medicine.
Type 2 diabetes
If you take insulin to manage type 2 diabetes, your healthcare professional might recommend a CGM. Or you may need blood sugar testing several times a day. The exact number of times depends on the type and amount of insulin you use. Often, testing is advised before meals and at bedtime if you take more than one shot of insulin a day. You may need to test only before breakfast and sometimes before dinner or at bedtime if you use an intermediate- or a long-acting insulin.
In general, you might need to test more often if you:
- Are sick.
- Have to drive a long distance.
- Change the way you eat or exercise.
You might not need to test your blood sugar every day if you manage type 2 diabetes with medicines that are not insulin. You also might not need to test daily if you manage the condition with diet and exercise alone.
Continuous glucose monitors (CGMs)
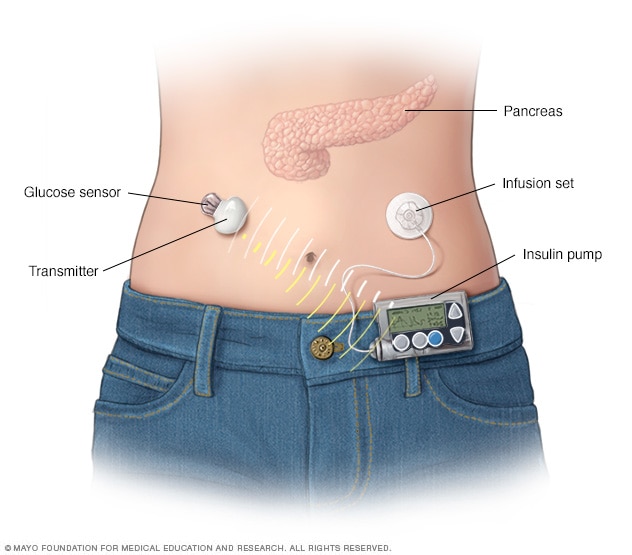
Continuous glucose monitor and insulin pump
A continuous glucose monitor, on the left, is a device that measures your blood sugar every few minutes using a sensor inserted under the skin. An insulin pump, attached to the pocket, is a device that's worn outside of the body with a tube that connects the reservoir of insulin to a catheter inserted under the skin of the abdomen. Insulin pumps are programmed to deliver specific amounts of insulin automatically and when you eat.
People living with diabetes may choose to use CGMs, especially people who have type 1 diabetes. CGMs measure blood sugar every few minutes. They use a device placed on the skin along with a sensor placed under the skin. These disposable sensors last for 10 days to two weeks before they need to be changed. Other types of implanted sensors can last up to 6 months.
CGMs include a wireless device worn on the body called a transmitter. The transmitter sends information from the sensor to a program that lets you view your blood sugar level. The program is viewed on a receiver, a smartphone or an insulin pump.
Some CGMs show your blood sugar reading at all times. They often include an alarm that goes off if your blood sugar goes up or down too quickly. Other CGMs require that you check your blood sugar by running the receiver over the sensor. You may need to do this every few hours. Some people have to do it more often.
With some CGMs, you still need to do finger-stick blood tests. These tests set the CGM. This is called calibration. The finger-stick blood tests also help keep the CGM readings precise. Check your device's user's guide to learn if you need to do finger-stick blood tests, and if so, how often.
Wine might make some CGM readings less precise. Some medicines also can have an effect on the readings, especially when used with older CGMs. Medicines that may affect blood sugar readings include:
- Acetaminophen (Tylenol, others).
- Albuterol (Proair HFA, Ventolin HFA, others).
- Aspirin.
- Atenolol (Tenoretic, Tenormin).
- Atorvastatin (Atorvaliq, Lipitor).
- Ethanol oleate (Ethamolin).
- Lisinopril (Zestril, Qbrelis).
- Vitamin C (Airborne, Emergen-C, others), also sold as ascorbic acid supplements.
Readings on newer CGMs don't seem to be affected by standard doses of acetaminophen — up to 1,000 milligrams for an adult. Newer CGM readings also don't appear to be affected by ascorbic acid supplements that are less than 500 milligrams.
If you need to take medicines that may affect the accuracy of the readings, check the package insert that comes with the sensor. Or talk to your healthcare professional. You may be told to double-check your CGM results with a standard blood sugar meter. Check with your healthcare professional about using a CGM if you are:
- Pregnant.
- On dialysis.
- Very ill.
These conditions may affect the blood sugar readings from a CGM.
Know your target range
Ask your healthcare team what the right blood sugar range is for you. Your healthcare professional works with you to set target blood-sugar test results based on factors that include:
- The type of diabetes you have.
- Your symptoms.
- Your age.
- How long you've lived with diabetes.
- Whether or not you are pregnant.
- Any health conditions you have that are related to diabetes.
- Your overall health and other medical conditions you have.
- The cost, complexity and frequency of side effects of the medicines used to treat diabetes.
The American Diabetes Association (ADA) tends to recommend the following target blood sugar levels. These targets are for most of the healthy people with diabetes who take medicines:
- Between 80 and 130 milligrams per deciliter (mg/dL) or 4.4 to 7.2 millimoles per liter (mmol/L) before meals.
- Less than 180 mg/dL (10.0 mmol/L) two hours after meals.
But the ADA notes that these goals often vary. Your goals depend on your age and your health. Tell your healthcare professional if your blood sugar is often higher or lower than your target range.
Some people will have slightly higher blood sugar goals, including those who:
- Are age 60 and older.
- Have other medical conditions such as heart, lung or kidney disease.
- Don't feel symptoms of low blood sugar. This is called hypoglycemia unawareness.
How to test blood sugar
A blood sugar meter is used to test blood sugar. The meter measures the amount of sugar in a small sample of blood. Most often, the blood comes from the side of the fingertip. Then the blood is placed on a disposable test strip. With certain CGMs, you still may need a blood sugar meter to set your CGM device daily.
Your healthcare professional or a certified diabetes care and education specialist can recommend a CGM device for you. They also can help you learn how to use your meter.
Follow the instructions that come with your blood sugar meter. In general, here's how the process works:
- Wash and dry your hands well. Food and other substances on your hands may lead to a reading that isn't correct.
- Place a test strip into your meter.
- Prick the side of your fingertip with the needle that comes with your test kit. That needle also is called a lancet.
- Touch and hold the edge of the test strip to the drop of blood.
- The meter displays your blood sugar level on a screen after a few seconds.
Some meters can test blood taken from another body part such as the forearm or palm. But these readings may not be as accurate as readings from the fingertips, especially after a meal or during exercise. Blood sugar levels change more often at these times. Using a body part other than the fingertips is not recommended when you set a CGM. That process also is called calibrating.
Record your results
Talk with your healthcare professional about how often you need to record your blood sugar results. The readings given by many devices can be sent to a computer or smart device.
If you write or type your results in a diary, be sure to record the:
- Date.
- Time.
- Test results.
- Any medicines and the dose you take.
- Diet and exercise information.
Bring your record of results with you to checkups with your healthcare professional. Ask what steps to take if you often get results that don't fall within the range of your target goals.
Help prevent problems with your meter
Blood sugar meters need to be used and cared for correctly. Follow these tips:
- Check the user's guide for your device directions. The way meters works may be different from one device to another.
- Use a blood sample size as directed in the user's guide.
- Use only test strips made for your meter.
- Store test strips as directed.
- Don't use expired test strips.
- Clean the device and run quality-control checks as directed.
- Bring the meter to your healthcare visits. This way, you can ask any questions. You also can ask your healthcare professional to watch you use your meter and make sure you use it correctly.