Achalasia
Achalasia is a disorder of the esophagus – the tube that carries food from your mouth to your stomach – that affects its ability to move food.
At the place where your esophagus and stomach meet, there is a muscular valve called the lower esophageal sphincter (LES). Your LES normally relaxes when you swallow so food can pass into your stomach. If you have achalasia, the muscular valve does not relax as well as it should, making it difficult for food to move into your stomach. In addition, your esophagus does not squeeze properly, which makes moving food through it more challenging.
Symptoms of Achalasia
Symptoms of achalasia include:
- Regurgitation of food, partially undigested food
- Chest pain
- Difficulty swallowing
- Persistent cough
- Unintentional weight loss
Causes of Achalasia
Achalasia occurs when the nerves of your esophagus don’t function correctly. The exact cause is unknown but may be triggered by viruses or autoimmune disease. Acalasia can occur at any age.

Learn More
For more information or to schedule an appointment with the St. Elizabeth Thoracic Surgery office, please call
(859) 301-2465.
Diagnosing Achalasia
- Physical exam – your doctor will give you a thorough physical exam to look for signs of malnutrition or anemia.
- Manometry – test to measure how your esophagus is working. This is the gold standard to diagnose achalasia.
- EGD or upper endoscopy – a way of looking inside your body that uses a special tube and a tiny camera.
- Esophagram – set of X-rays taken to examine your esophagus, stomach and small intestine.
- Barium swallow – uses barium to monitor movement through your esophagus, stomach and small intestine.
Treating Achalasia
The thoracic experts at St. Elizabeth Healthcare will review your health history and test results to develop a plan that addresses your specific health needs. The goal when treating achalasia is reducing the pressure of the lower esophageal valve muscle to allow food and liquids to pass more easily into your stomach.
Treatment may include:
- Botox – uses an endoscope (a thin tube with a camera) to inject Botox into your lower esophageal valve to help it relax and improve your ability to swallow. Botox is the least invasive treatment for achalasia, but it doesn’t last as long as the other options. The medication’s effectiveness wears off within a few months of the injection. Using Botox repeatedly may cause scarring that could make future treatment more difficult. It is considered a temporary solution for achalasia.
- Balloon dilatation – an endoscopic procedure that uses a specially designed balloon to stretch your lower esophageal valve. It is a good option if surgery is considered too high risk, but it does not last as long. Repeat procedures may be necessary, which is the main difference between balloon dilatation and Heller myotomy.
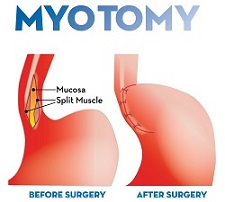
Heller myotomy – minimally invasive surgery done with very small tools attached to a robotic arm controlled by your surgeon. Your esophagus valve is opened permanently with precise cuts of your lower esophageal valve, which reduces pressure and allows your food to pass more easily into your stomach. The procedure is usually paired with an anti-reflux procedure known as partial fundoplication to prevent uncontrolled reflux. Heller myotomy is the gold standard for achalasia treatment.
When you have achalasia, the aim of treatment is to treat symptoms of swallowing and help reduce complications which include aspiration, pneumonia, weight loss and malnutrition. If left untreated long term, achalasia can increase your risk for cancer of the esophagus.
Schedule an Appointment Today
Call Us to Schedule a Visit
For more information or to schedule an appointment with the St. Elizabeth Thoracic Surgery office, please call
(859) 301-2465.