Salivary Gland Cancer
St. Elizabeth Healthcare offers specialized expertise for head and neck cancers — even rare types like salivary gland cancer. Our team provides the latest medical treatments and supportive cancer care for your health and wellbeing.
Salivary gland cancer starts in the organs in your mouth and throat that produce saliva, or spit. Salivary gland cancer is rare and makes up only 6% to 8% of all head and neck cancers in the U.S. The most common types are

Make an appointment
For more information, please contact your oncologist or call (859) 301-4000.
Causes and Risk Factors of Salivary Gland Cancer
Medical experts don’t know what causes salivary gland cancer. Certain gene mutations may play a role in increasing your risk.
People of any age can develop salivary cancer, though it becomes more common as people get older.
These factors can increase your risk of salivary gland cancer:
- Older age.
- Radiation exposure near the head or neck.
- Tobacco use, including smoking, vaping and chewing.
Symptoms of Salivary Gland Cancer
Because of their location, salivary gland tumors can cause symptoms in your face, mouth and throat.
Possible symptoms of salivary gland cancer include:
- Change in size or shape in one side of your face or neck.
- Difficulty opening your mouth or swallowing.
- Lump or swelling in your cheek, jaw, mouth or neck.
- Numbness or weakness in part of your cheek, jaw, mouth or neck.
- Persistent pain in your cheek, jaw, mouth or neck.
Benign (noncancerous) salivary gland tumors and other conditions can also cause these symptoms. Tell your primary care provider or dentist if you notice any of these signs.
Diagnosing Salivary Gland Cancer
We start with the right diagnosis to build your personalized treatment plan. First, your provider will give you a physical exam and review your health history.
We use a range of tests to diagnose salivary gland cancer, including:
Treating Salivary Gland Cancer
Your personalized treatment plan will include the latest medical techniques for salivary gland cancer. Our cancer care team coordinates treatment and support for your health and well being.
It’s important to quit using tobacco (smoking, vaping or chewing) before you begin treatment for salivary gland cancer. Using tobacco will make the treatments less effective, lead to more side effects and block your body’s ability to heal.
Depending on the stage of your cancer and whether it has spread, your treatment may include:
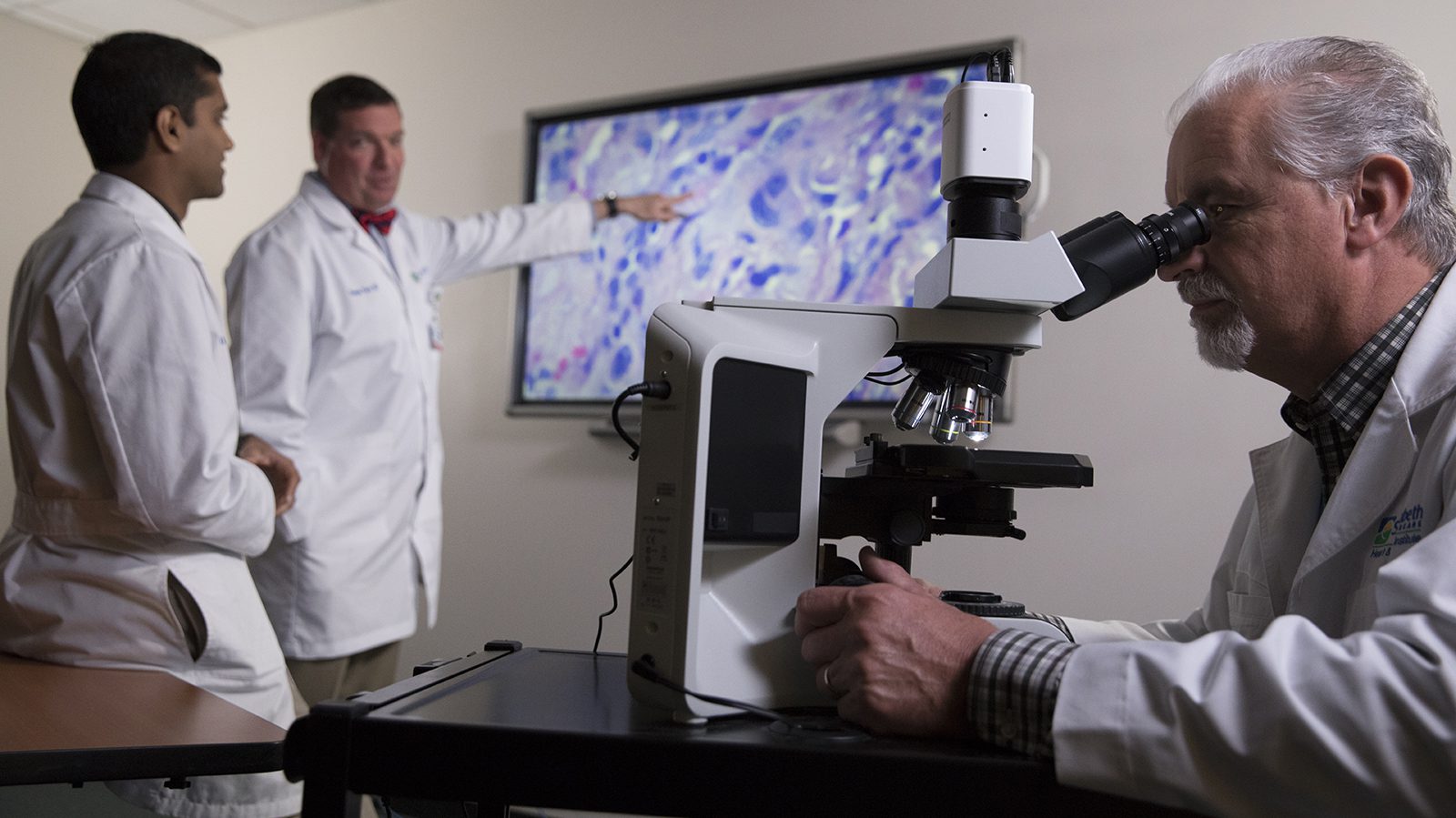
Your Cancer Care Team
You’re not alone during your cancer care journey. In fact, you have an entire team of dedicated specialists at St. Elizabeth Healthcare. Together, they create your treatment plan and support your well being.
Your cancer care team includes:
- Medical oncologists (cancer care physicians) specializing in immunotherapy and precision medicine.
- Surgical oncologists and thoracic surgeons.
- Radiation oncologists.
- Interventional radiologists.
- Pain management specialists.
- Genetic counselors.
- Pathologists.
- Nutritionists.
- Pharmacists.
- Nurses.
- Support staff.