Thoracic aortic aneurysm
Updated: 2023-04-25
Overview
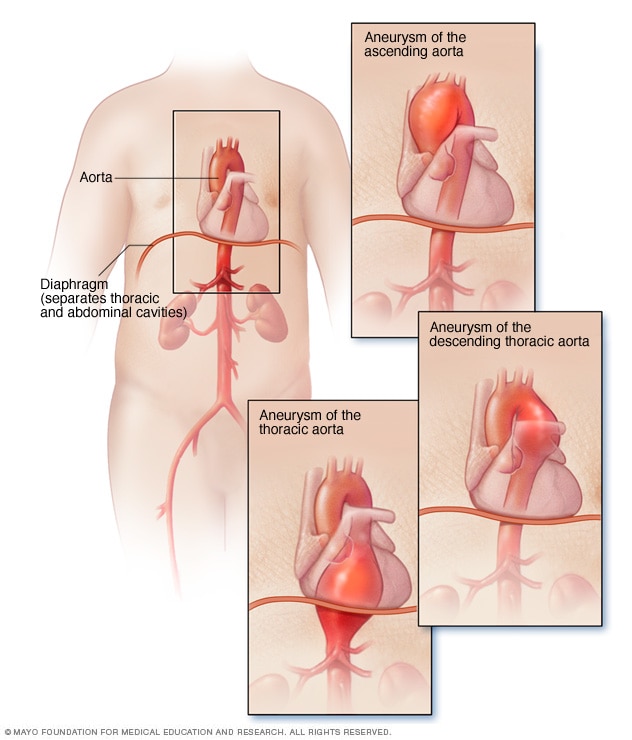
Thoracic aortic aneurysm
A thoracic aortic aneurysm is a weakened area in the upper part of the aorta — the major blood vessel that feeds blood to the body. Aneurysms can develop anywhere in the aorta.
A thoracic aortic aneurysm is a weakened area in the body's main artery in the chest. The body's main artery is called the aorta. When the aortic wall is weak, the artery may widen. When the vessel is significantly widened, it's called an aneurysm.
A thoracic aortic aneurysm also is called a thoracic aneurysm.
Treatment of a thoracic aortic aneurysm may vary from regular health checkups to emergency surgery. The type of treatment depends on the cause, size and growth rate of the thoracic aortic aneurysm.
Complications of a thoracic aortic aneurysm include rupture of the aorta or a life-threatening tear between the layers of the aorta's wall. The tear is called an aortic dissection. Rupture or dissection can lead to sudden death.
Thoracic aortic aneurysms are less common than aneurysms that form in the lower part of the aorta, called abdominal aortic aneurysms.
Symptoms
Thoracic aortic aneurysms often grow slowly. There are usually no symptoms, making them difficult to detect. Many start small and stay small. Others grow bigger over time. How quickly a thoracic aortic aneurysm may grow is difficult to predict.
As a thoracic aortic aneurysm grows, symptoms may include:
- Back pain.
- Cough.
- Weak, scratchy voice.
- Shortness of breath.
- Tenderness or pain in the chest.
Symptoms that a thoracic aortic aneurysm has ruptured or dissected include:
- Sharp, sudden pain in the upper back that spreads downward.
- Pain in the chest, jaw, neck or arms.
- Difficulty breathing.
- Low blood pressure.
- Loss of consciousness.
- Shortness of breath.
- Trouble swallowing.
Some aneurysms may never rupture or lead to dissection.
When to see a doctor
Most people with aortic aneurysms don't have symptoms unless a dissection or rupture occurs. An aortic dissection or aneurysm rupture is a medical emergency. Call 911 or your local emergency number for immediate help.
Causes
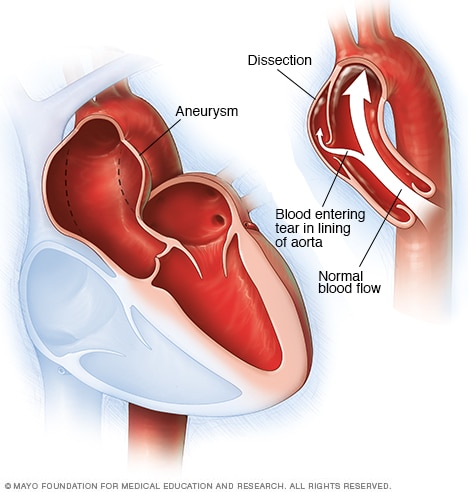
Aortic aneurysm and aortic dissection
An aortic aneurysm occurs when a weak spot in the wall of the aorta begins to bulge, as shown in the image on the left. An aneurysm can occur anywhere in the aorta. Having an aortic aneurysm increases the risk of a tear in the aortic lining, called a dissection, as shown in the image on the right.
Aortic aneurysms can develop anywhere in the body's main artery, called the aorta. The aorta runs from the heart through the chest and belly area. When an aneurysm occurs in the chest, it's called a thoracic aortic aneurysm.
If an aneurysm forms between the upper and lower parts of the aorta, it's called a thoracoabdominal aneurysm.
A thoracic aneurysm may be round or tube-shaped.
Aneurysms can occur anywhere in the thoracic aorta, including near the heart, in the aortic arch and in the lower part of the thoracic aorta.
Causes of thoracic aortic aneurysms may include:
- Hardening of the arteries, called atherosclerosis. Plaque buildup on the artery walls causes the arteries to become less flexible. Additional pressure can cause the arteries to weaken and widen. High blood pressure and high cholesterol increase the risk of atherosclerosis. This is more common in older people.
-
Genetic conditions. Aortic aneurysms in younger people often have a genetic cause. Marfan syndrome, a genetic condition that affects the connective tissue in the body, may cause weakness in the wall of the aorta.
Other genetic conditions linked to aortic aneurysm and dissection and rupture include vascular Ehlers-Danlos, Loeys-Dietz and Turner syndromes.
- Blood vessel inflammation. Conditions that involve blood vessel inflammation, such as giant cell arteritis and Takayasu arteritis, are associated with thoracic aortic aneurysms.
- Irregular aortic valve. The aortic valve is between the lower left heart chamber and the aorta. People who are born with an aortic valve that has only two flaps instead of three have an increased risk of a thoracic aneurysm.
- Untreated infection. Though rare, it's possible to develop a thoracic aortic aneurysm if you've had an untreated infection, such as syphilis or salmonella.
- Traumatic injury. Rarely, some people who are injured in falls or motor vehicle crashes develop thoracic aortic aneurysms.
Aortic emergencies
In aortic dissection, a tear occurs in the wall of the aorta. This causes bleeding into and along the aortic wall. Sometimes the bleeding moves completely outside the aorta. When this happens, it's called an aortic rupture.
An aortic dissection is a potentially life-threatening emergency, depending on where in the aorta it occurs. It's important to treat an aortic aneurysm to try to prevent dissection. If dissection occurs, people can still be treated with surgery. However, they typically have a higher risk of complications.
Risk factors
Thoracic aortic aneurysm risk factors include:
- Age. Growing older increases the risk of aortic aneurysms. Thoracic aortic aneurysms occur most often in people age 65 and older.
- Tobacco use. Smoking and using tobacco greatly increases the risk of an aortic aneurysm.
- High blood pressure. Increased blood pressure damages the blood vessels in the body, raising the risk of an aneurysm.
- Buildup of plaques in the arteries. The buildup of fat and other substances in the blood can damage the lining of a blood vessel, increasing the risk of an aneurysm. This is a more common risk in older people.
- Family history. Having a parent, brother, sister or child with an aortic aneurysm increases the risk of an aortic aneurysm and rupture. You may develop aneurysms at a younger age.
- Genetic conditions. If you have Marfan syndrome or a related condition, such as Loeys-Dietz syndrome or vascular Ehlers-Danlos syndrome, you have a significantly higher risk of a thoracic aortic aneurysm. The risk also is increased for an aortic or other blood vessel dissection or rupture.
- Bicuspid aortic valve. Having an aortic valve with two cusps instead of three increases the risk of aortic aneurysm.
Complications
Tears in the wall of the aorta and rupture of the aorta are the main complications of thoracic aortic aneurysm. However, some small and slow-growing aneurysms may never rupture. In general, the larger the aneurysm, the greater the risk of rupture.
Complications of a thoracic aortic aneurysm and rupture can include:
- Life-threatening bleeding inside the body. This is called internal bleeding. Emergency surgery is required to try to prevent death.
- Blood clots. Small blood clots can develop in the area of the aortic aneurysm. If a blood clot breaks loose from the inside wall of an aneurysm, it can block a blood vessel elsewhere in the body. This can possibly cause serious complications.
- Stroke. Signs and symptoms of stroke include weakness of or an inability to move one side of the body. It may be difficult to speak.
Prevention
Keeping the blood vessels as healthy as possible is important in preventing an aneurysm. A health care provider may recommend these heart-healthy strategies:
- Don't smoke or use tobacco products.
- Keep blood pressure and cholesterol levels under control.
- Get regular exercise.
- Reduce cholesterol and fat in the diet.
There are no medicines to prevent an aortic aneurysm. However, medicines may be used to treat high blood pressure, high cholesterol and other conditions linked to aneurysm. Proper management of such conditions may lower the risk of thoracic aortic aneurysm complications.
Screening and genetic testing
Conditions that cause a thoracic aortic aneurysm may run in families. A health care provider may recommend screening if a first-degree relative — such as a parent, brother, sister, son or daughter — has a genetic disease such as Marfan syndrome or another condition linked to thoracic aortic aneurysms.
Screening means you have regular imaging tests, usually an echocardiogram, to check for an aneurysm. If an ultrasound of the heart shows an enlarged aorta or an aneurysm, another imaging test is usually done within 6 to 12 months to make sure it hasn't grown.
Genetic testing also may be recommended if you have a family history of aortic aneurysms, particularly if you're considering pregnancy.
Diagnosis
Thoracic aortic aneurysms are often found when an imaging test is done for a different reason.
If you have symptoms of a thoracic aortic aneurysm, your health care provider may ask about your family's medical history. Some aneurysms can run in families.
Tests
Imaging tests can be used to confirm or screen for a thoracic aortic aneurysm. Tests may include:
- Echocardiogram. This test uses sound waves to show how blood moves through the heart and blood vessels, including the aorta. An echocardiogram may be used to diagnose or screen for thoracic aortic aneurysms. If a standard echocardiogram doesn't provide enough information about the aorta, a transesophageal echocardiogram may be done to get a better view. For this type of echocardiogram, a flexible tube containing an ultrasound wand is guided down the throat and into the tube connecting the mouth to the stomach.
- Computerized tomography (CT). CT uses X-rays to create cross-sectional images of the body, including the aorta. It can show the size and shape of an aneurysm. During a CT scan, you typically lie on a table inside a doughnut-shaped X-ray machine. Dye, called contrast, may be given by IV to help the arteries show up more clearly on the X-ray.
- Cardiac magnetic resonance imaging (MRI). A cardiac MRI uses magnetic fields and radio waves to create detailed images of the heart and aorta. It can help diagnose an aneurysm and show its size and location. In this test, you typically lie on a table that slides into a tunnel. Dye may be given by IV to help blood vessels show up more clearly on the images. This test doesn't use radiation. It may be an option to CT scans for people who need frequent aneurysm imaging tests.
Treatment
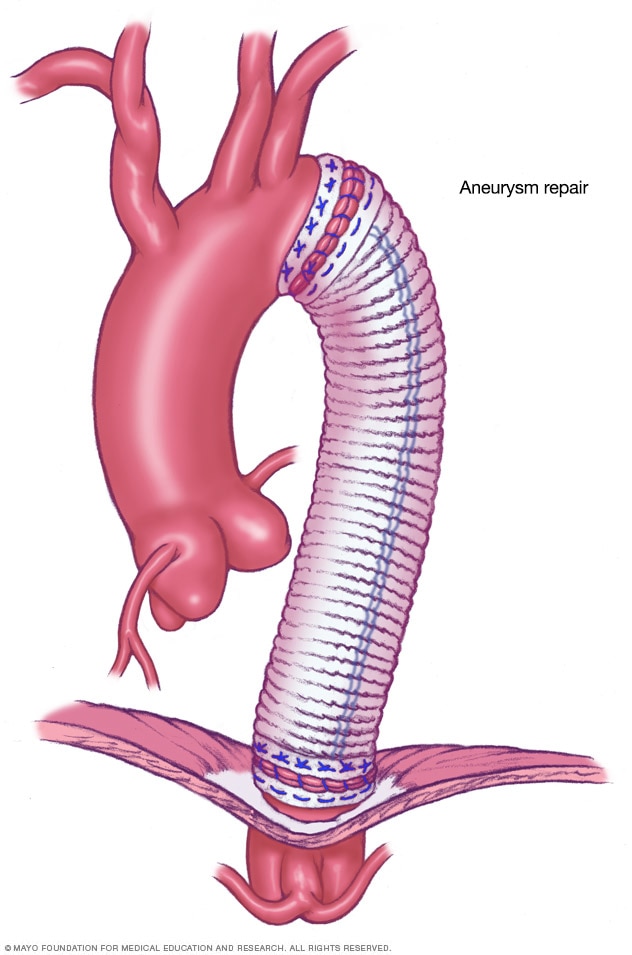
Open-chest surgery for thoracic aortic aneurysm
Open-chest surgery to repair a thoracic aortic aneurysm involves removing the damaged part of the aorta. The damaged part is replaced with a synthetic tube, called a graft, which is sewn into place.
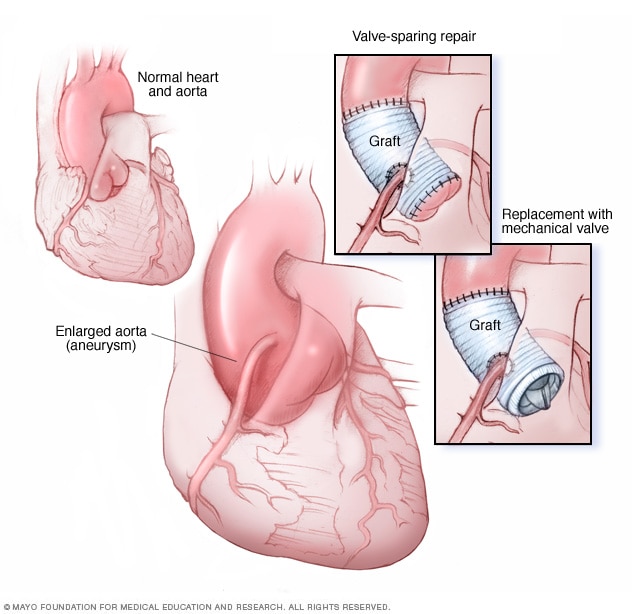
Ascending aortic root aneurysm procedure
Aortic root surgery is generally done in two ways. Valve-sparing aortic root repair (top-right image) replaces the enlarged section of the aorta with an artificial tube, called a graft. The aortic valve stays in place. In aortic valve and aortic root replacement (bottom-right image), the aortic valve and a part of the aorta are removed. A graft replaces the section of the aorta. A mechanical or biological valve replaces the valve.
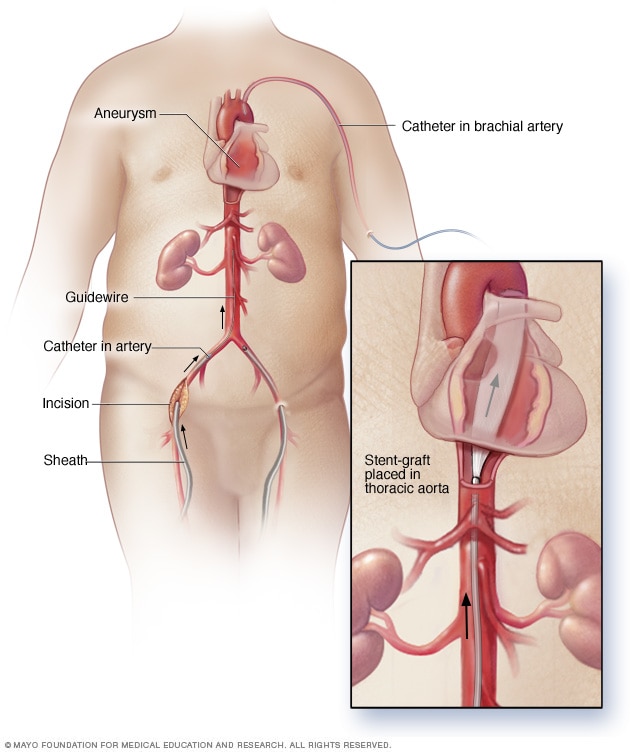
Endovascular repair for thoracic aortic aneurysm
In endovascular thoracic aortic aneurysm repair, the surgeon inserts a thin, flexible tube called a catheter through an artery in the groin area and guides it to the aorta. A metal mesh tube called a graft is on the end of the catheter. The graft is placed at the aneurysm site. It's secured with small hooks or pins. The graft strengthens the weakened section of the aorta to prevent rupture of the aneurysm.
The goal of treatment for a thoracic aortic aneurysm is to prevent the aneurysm from growing and rupturing. Treatment depends on the aneurysm's size and how fast it's growing.
Treatment for thoracic aortic aneurysm may include:
- Regular health checkups, sometimes called watchful waiting.
- Medicines.
- Surgery.
If your thoracic aortic aneurysm is small, your health care provider may recommend medicine and imaging tests to watch the aneurysm. Other health conditions will be treated and managed.
Usually, you'll have an echocardiogram, CT or magnetic resonance angiography (MRA) scan at least six months after your aneurysm is diagnosed. An imaging test also may be done at regular follow-up exams. How often you have these tests done depends on the cause and size of the aneurysm, and how fast it's growing.
Medications
Medicines may be prescribed to treat high blood pressure and high cholesterol.
These medicines could include:
- Beta blockers. These medicines lower blood pressure by slowing the heart rate. They may reduce how fast the aorta is widening in people with Marfan syndrome.
- Angiotensin 2 receptor blockers. These medicines may be used if beta blockers can't be taken or if they don't adequately control blood pressure. They are often recommended for people who have Loeys-Dietz syndrome even if they don't have high blood pressure. Examples of angiotensin 2 receptor blockers include losartan (Cozaar), valsartan (Diovan) and olmesartan (Benicar).
- Statins. These medicines can help lower cholesterol, which can help reduce blockages in the arteries and reduce the risk of aneurysm complications. Examples of statins include atorvastatin (Lipitor), lovastatin (Altoprev), simvastatin (Zocor, FloLipid) and others.
If you smoke or chew tobacco, it's important that you quit. Using tobacco can worsen an aneurysm and overall health.
Surgery
Surgery is generally recommended for thoracic aortic aneurysms about 1.9 to 2.4 inches (about 5 to 6 centimeters) and larger. Surgery may be recommended for smaller aneurysms if you have a family history of aortic dissection or a condition linked to aortic aneurysm, such as Marfan syndrome.
Most people with a thoracic aortic aneurysm have open-chest surgery, but sometimes a less invasive procedure called endovascular surgery can be done.
The type of surgery done depends on the specific health condition and the location of the thoracic aortic aneurysm.
- Open-chest surgery. This surgery generally involves removing part of the aorta damaged by the aneurysm. The section of aorta is replaced with a synthetic tube, called a graft, which is sewn into place. Full recovery may take a month or more.
- Aortic root surgery. This type of open-chest surgery is done to treat an enlarged section of the aorta to prevent a rupture. Aortic aneurysms near the aortic root may be related to Marfan syndrome and other related conditions. A surgeon removes part of the aorta and sometimes the aortic valve. A graft replaces the removed section of the aorta. The aortic valve may be replaced with a mechanical or biological valve. If the valve is not removed, the surgery is called valve-sparing aortic root repair.
-
Endovascular aortic aneurysm repair (EVAR). The surgeon inserts a thin, flexible tube into a blood vessel, usually in the groin, and guides it to the aorta. A metal mesh tube, called a graft, on the end of the catheter is placed at the aneurysm site. Small hooks or pins hold it in place. The graft reinforces the weakened section of the aorta to prevent rupture of the aneurysm. This catheter-based procedure may allow a faster recovery.
EVAR can't be done on everyone. Ask your health care provider whether it's right for you. After EVAR, you'll need regular imaging tests to check the graft for leakage.
- Emergency surgery. A ruptured thoracic aortic aneurysm requires emergency open-chest surgery. This type of surgery is risky and has a high chance of complications. That's why it's important to identify and treat thoracic aortic aneurysms before they rupture with lifelong health checkups and appropriate preventive surgery.
Lifestyle and home remedies
If you have a thoracic aortic aneurysm, your health care provider may tell you not to do heavy lifting and some vigorous physical activities. Such activities can increase blood pressure, putting additional pressure on your aneurysm.
If you want to participate in a particular activity, your health care provider may recommend an exercise stress test to see how exercise affects your blood pressure. Moderate physical activity is generally healthy for you.
Stress also can raise blood pressure, so find ways to help reduce emotional stress. Getting more exercise and practicing mindfulness are some ways to reduce stress.
Coping and support
Some people with a thoracic aortic aneurysm or related conditions may feel anxious, worried or depressed. You may find that connecting with others who have experienced similar situations may be helpful. Talk to your health care provider about support groups in your area.
Preparing for an appointment
If you think you may have a thoracic aortic aneurysm or are worried about your aneurysm risk because of a strong family history, make an appointment with your care provider. If an aneurysm is found early, treatment may be easier and more effective.
If you're being screened for an aortic aneurysm, your health care provider will likely ask if anyone in your family has ever had an aortic aneurysm, so have that information ready.
Because appointments can be brief and there's often a lot to discuss, it's a good idea to be prepared for your appointment. Here's some information to help you get ready for your appointment, and what to expect from your health care provider.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance. For an echocardiogram, for example, you may need to avoid food or drinks for a period beforehand.
- Write down any symptoms you're having, including any that may seem unrelated to a thoracic aortic aneurysm.
- Write down important personal information, including a family history of heart disease, aneurysms or connective tissue disease.
- Make a list of all medicines, vitamins or supplements that you take. Include dosages.
- Take a family member or friend along, if possible. Sometimes it can be difficult to remember the information provided to you during an appointment. Someone who goes with you may remember something that you missed or forgot.
- Be prepared to discuss your diet, exercise habits and tobacco use. If you don't already follow a diet or exercise routine, tell your care provider about any challenges you might face in getting started. Be sure to tell your health care provider if you're a current or former smoker.
- Send imaging reports and bring records. It's helpful if you can send imaging reports to your health care provider in advance and bring your medical records.
- Write down questions to ask your health care provider.
Your time with your health care provider is limited, so preparing a list of questions will help you make the most of your time together. List your questions from most important to least important in case time runs out. For an aortic aneurysm, some basic questions to ask your health care provider include:
- What kinds of tests will I need to confirm a thoracic aortic aneurysm?
- What size is my aneurysm?
- What treatments are available, and which do you recommend for me?
- What's an appropriate level of physical activity?
- Do I need to change my diet?
- How often should I be screened for an aneurysm?
- Should I tell other family members to be screened for an aneurysm?
- I have other health conditions. How can I best manage these conditions together?
- Is there a generic alternative to the medicine you're prescribing me?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend visiting for more information?
In addition to the questions that you've prepared to ask your health care provider, don't hesitate to ask additional questions during your appointment.
What to expect from your doctor
Your health care provider is likely to ask you several questions. Being ready to answer them may reserve time to go over any points you want to spend more time on. Your health care provider may ask:
- When did you first begin having symptoms?
- Do your symptoms come and go, or do you have them all the time?
- How severe are your symptoms?
- Do you have a family history of aneurysms or genetic diseases, such as Marfan syndrome?
- Have you ever smoked?
- Have you ever been told you have high blood pressure?
- Does anything improve your symptoms?
- What, if anything, appears to worsen your symptoms?
What you can do in the meantime
It's never too early to make healthy lifestyle changes, such as quitting smoking, eating healthy foods and getting more exercise. Taking these steps can help prevent thoracic aortic aneurysm and its complications.
If you're diagnosed with a thoracic aortic aneurysm, ask how often you should visit your health care provider for follow-up appointments.