Sjogren's syndrome
Updated: 2022-08-02
Overview
Sjogren's (SHOW-grins) syndrome is a disorder of your immune system identified by its two most common symptoms — dry eyes and a dry mouth.
The condition often accompanies other immune system disorders, such as rheumatoid arthritis and lupus. In Sjogren's syndrome, the mucous membranes and moisture-secreting glands of your eyes and mouth are usually affected first — resulting in decreased tears and saliva.
Although you can develop Sjogren's syndrome at any age, most people are older than 40 at the time of diagnosis. The condition is much more common in women. Treatment focuses on relieving symptoms.
Symptoms
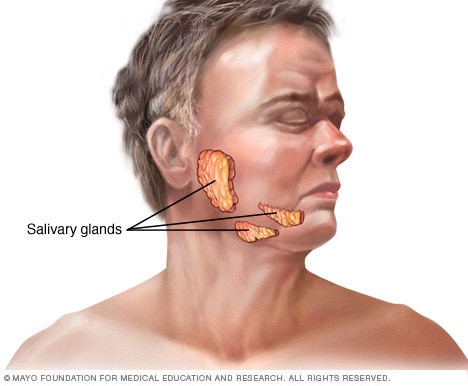
Salivary glands
There are three pairs of major salivary glands. These glands are the parotid, sublingual and submandibular glands. Each gland has its own tube, called a duct, leading from the gland to the mouth.
The two main symptoms of Sjogren's syndrome are:
- Dry eyes. Your eyes might burn, itch or feel gritty — as if there's sand in them.
- Dry mouth. Your mouth might feel like it's full of cotton, making it difficult to swallow or speak.
Some people with Sjogren's syndrome also have one or more of the following:
- Joint pain, swelling and stiffness
- Swollen salivary glands — particularly the set located behind your jaw and in front of your ears
- Skin rashes or dry skin
- Vaginal dryness
- Persistent dry cough
- Prolonged fatigue
Causes
Sjogren's syndrome is an autoimmune disorder. Your immune system mistakenly attacks your body's own cells and tissues.
Scientists aren't certain why some people develop Sjogren's syndrome. Certain genes put people at higher risk of the disorder, but it appears that a triggering mechanism — such as infection with a particular virus or strain of bacteria — is also necessary.
In Sjogren's syndrome, your immune system first targets the glands that make tears and saliva. But it can also damage other parts of your body, such as:
- Joints
- Thyroid
- Kidneys
- Liver
- Lungs
- Skin
- Nerves
Risk factors
Sjogren's syndrome typically occurs in people with one or more known risk factors, including:
- Age. Sjogren's syndrome is usually diagnosed in people older than 40.
- Sex. Women are much more likely to have Sjogren's syndrome.
- Rheumatic disease. It's common for people who have Sjogren's syndrome to also have a rheumatic disease — such as rheumatoid arthritis or lupus.
Complications
The most common complications of Sjogren's syndrome involve your eyes and mouth.
- Dental cavities. Because saliva helps protect the teeth from the bacteria that cause cavities, you're more prone to developing cavities if your mouth is dry.
- Yeast infections. People with Sjogren's syndrome are much more likely to develop oral thrush, a yeast infection in the mouth.
- Vision problems. Dry eyes can lead to light sensitivity, blurred vision and corneal damage.
Less common complications might affect:
- Lungs, kidneys or liver. Inflammation can cause pneumonia, bronchitis or other problems in your lungs; lead to problems with kidney function; and cause hepatitis or cirrhosis in your liver.
- Lymph nodes. A small percentage of people with Sjogren's syndrome develop cancer of the lymph nodes (lymphoma).
- Nerves. You might develop numbness, tingling and burning in your hands and feet (peripheral neuropathy).
Diagnosis
Sjogren's syndrome can be difficult to diagnose because the signs and symptoms vary from person to person and can be similar to those caused by other diseases. Side effects of a number of medications also mimic some signs and symptoms of Sjogren's syndrome.
Tests can help rule out other conditions and help pinpoint a diagnosis of Sjogren's syndrome.
Blood tests
Your doctor might order blood tests to check for:
- Levels of different types of blood cells
- Presence of antibodies common in Sjogren's syndrome
- Evidence of inflammatory conditions
- Indications of problems with your liver and kidneys
Eye tests
Your doctor can measure the dryness of your eyes with a test called a Schirmer tear test. A small piece of filter paper is placed under your lower eyelid to measure your tear production.
A doctor specializing in the treatment of eye disorders (ophthalmologist) might also examine the surface of your eyes with a magnifying device called a slit lamp. He or she may place drops in your eye that make it easier to see damage to your cornea.
Imaging
Certain imaging tests can check the function of your salivary glands.
- Sialogram. This special X-ray can detect dye that's injected into the salivary glands in front of your ears. This procedure shows how much saliva flows into your mouth.
- Salivary scintigraphy. This nuclear medicine test involves the injection into a vein of a radioactive isotope, which is tracked over an hour to see how quickly it arrives in all your salivary glands.
Biopsy
Your doctor might also do a lip biopsy to detect the presence of clusters of inflammatory cells, which can indicate Sjogren's syndrome. For this test, a sliver of tissue is removed from salivary glands in your lip and examined under a microscope.
Treatment
Treatment for Sjogren's syndrome depends on the parts of the body affected. Many people manage the dry eye and dry mouth of Sjogren's syndrome by using over-the-counter eyedrops and sipping water more frequently. But some people need prescription medications, or even surgical procedures.
Medications
Depending on your symptoms, your doctor might suggest medications that:
- Decrease eye inflammation. Prescription eyedrops such as cyclosporine (Restasis) or lifitegrast (Xiidra) may be recommended by your eye doctor if you have moderate to severe dry eyes.
- Increase production of saliva. Drugs such as pilocarpine (Salagen) and cevimeline (Evoxac) can increase the production of saliva, and sometimes tears. Side effects can include sweating, abdominal pain, flushing and increased urination.
- Address specific complications. If you develop arthritis symptoms, you might benefit from nonsteroidal anti-inflammatory drugs (NSAIDs) or other arthritis medications. Yeast infections in the mouth should be treated with antifungal medications.
- Treat systemwide symptoms. Hydroxychloroquine (Plaquenil), a drug designed to treat malaria, is often helpful in treating Sjogren's syndrome. Drugs that suppress the immune system, such as methotrexate (Trexall), also might be prescribed.
Surgery
A minor procedure to seal the tear ducts that drain tears from your eyes (punctal occlusion) might help relieve your dry eyes. Collagen or silicone plugs are inserted into the ducts to help preserve your tears.
Lifestyle and home remedies
Many Sjogren's syndrome symptoms respond well to self-care measures.
To relieve dry eyes:
-
Use artificial tears, an eye lubricant or both. Artificial tears — in eyedrop form — and eye lubricants — in eyedrop, gel or ointment form — help relieve the discomfort of dry eyes. You don't have to apply eye lubricants as often as artificial tears. Because of their thicker consistency, eye lubricants can blur your vision and collect on your eyelashes, so you might want to use them only overnight.
Your doctor might recommend artificial tears without preservatives, which can irritate the eyes of people with dry eye syndrome.
- Increase humidity. Increasing the indoor humidity and reducing your exposure to blowing air can help keep your eyes and mouth from getting uncomfortably dry. For example, avoid sitting in front of a fan or air conditioning vent, and wear goggles or protective eyewear when you go outdoors.
To help with dry mouth:
- Don't smoke. Smoking can irritate and dry out your mouth.
- Increase your fluid intake. Take sips of fluids, particularly water, throughout the day. Avoid drinking coffee or alcohol since they can worsen dry mouth symptoms. Also avoid acidic beverages such as colas and some sports drinks because the acid can harm the enamel of your teeth.
- Stimulate saliva flow. Sugarless gum or citrus-flavored hard candies can boost saliva flow. Because Sjogren's syndrome increases your risk of dental cavities, limit sweets, especially between meals.
- Try artificial saliva. Saliva replacement products often work better than plain water because they contain a lubricant that helps your mouth stay moist longer. These products come as a spray or lozenge.
- Use nasal saline spray. A nasal saline spray can help moisturize and clear nasal passages so that you can breathe freely through your nose. A dry, stuffy nose can increase mouth breathing.
Oral health
Dry mouth increases your risk of dental cavities and tooth loss. To help prevent those types of problems:
- Brush your teeth and floss after every meal
- Schedule regular dental appointments, at least every six months
- Use daily topical fluoride treatments and antimicrobial mouthwashes
Other areas of dryness
If dry skin is a problem, avoid hot water when you bathe and shower. Pat your skin — don't rub — with a towel, and apply moisturizer when your skin is still damp. Use rubber gloves when doing dishes or housecleaning. Vaginal moisturizers and lubricants help women who have vaginal dryness.
Preparing for an appointment
Depending on your symptoms, you might start by seeing your family doctor, dentist or eye doctor. But you might eventually be referred to a doctor who specializes in the treatment of arthritis and other inflammatory conditions (rheumatologist).
What you can do
Make a list that includes:
- Detailed descriptions of your symptoms and when they began
- Information about your current and past medical problems
- Information about your parents' or siblings' medical history
- All medications and dietary supplements you take, including doses
- Questions you want to ask the doctor
For Sjogren's syndrome, basic questions include:
- What is likely causing my symptoms?
- Are there other possible causes?
- What tests do I need?
- What treatment approach do you recommend?
- How soon can I expect my symptoms to improve with treatment?
- Am I at risk of long-term complications from this condition?
- I have other health conditions. How can I best manage them together?
- Do you have brochures or other printed materials that I can have? What websites do you recommend?
What to expect from your doctor
Your doctor is likely to ask you a number of questions, including:
- Do your symptoms follow a pattern — worsening throughout the day or when you go outdoors?
- Do you have chronic conditions such as high blood pressure or arthritis?
- Have you recently started new medications?
- Do any close relatives have rheumatoid arthritis, lupus or a similar disease?