Glioblastoma
Updated: 2024-12-19
Overview
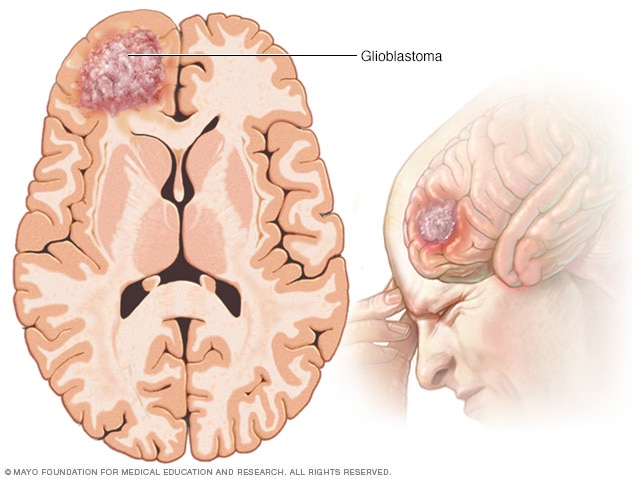
Glioblastoma
Glioblastoma is a type of cancer that starts in cells called astrocytes that support nerve cells. It can form in the brain or spinal cord.
Glioblastoma is a type of cancer that starts as a growth of cells in the brain or spinal cord. It grows quickly and can invade and destroy healthy tissue. Glioblastoma forms from cells called astrocytes that support nerve cells.
Glioblastoma can happen at any age. But it tends to happen more often in older adults. Glioblastoma symptoms may include headaches that keep getting worse, nausea and vomiting, blurred or double vision, trouble speaking, altered sense of touch, and seizures. There also may be trouble with balance, coordination, and moving parts of the face or body.
There's no cure for glioblastoma. Treatments might slow cancer growth and reduce symptoms.
Symptoms
Signs and symptoms of glioblastoma may include:
- Headache, particularly one that hurts the most in the morning.
- Nausea and vomiting.
- Confusion or a decline in brain function, such as problems with thinking and understanding information.
- Memory loss.
- Personality changes or irritability.
- Vision changes, such as blurred vision, double vision or loss of peripheral vision.
- Speech difficulties.
- Trouble with balance or coordination.
- Muscle weakness in the face, arms or legs.
- Reduced sensation of touch.
- Seizures, especially in someone who hasn't had seizures before.
When to see a doctor
Make an appointment with a doctor or other healthcare professional if you have any signs or symptoms that worry you.
Causes
The cause of most glioblastomas isn't known.
Glioblastoma happens when cells in the brain or spinal cord develop changes in their DNA. Healthcare professionals sometimes call these changes mutations or variations. A cell's DNA holds the instructions that tell a cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
The cancer cells form a mass called a tumor. The tumor can grow to press on nearby nerves and parts of the brain or spinal cord. This leads to glioblastoma symptoms and can cause complications. The tumor can grow to invade and destroy healthy body tissue.
Risk factors
Factors that can increase the risk of glioblastoma include:
- Getting older. Glioblastomas are most common in older adults. But glioblastoma can happen at any age.
- Being exposed to radiation. People who have been exposed to a type of radiation called ionizing radiation have an increased risk of glioblastoma. One example of ionizing radiation is radiation therapy used to treat cancer.
- Inherited syndromes that increase cancer risk. In some families, DNA changes passed from parents to children may increase the risk of glioblastoma. Inherited syndromes may include Lynch syndrome and Li-Fraumeni syndrome. Genetic testing can detect these syndromes.
Researchers haven't found anything you can do to prevent glioblastoma.
Diagnosis
Tests and procedures used to diagnose glioblastoma include:
- Neurological exam. This type of exam checks vision, hearing, balance, coordination, strength and reflexes. Problems in one or more of these areas might give clues about the part of the brain the glioblastoma affects.
- Imaging tests. Imaging tests can help find the location and size of a glioblastoma. MRI is the imaging test used most often. Sometimes you have an injection of dye in a vein before your MRI. This helps create better pictures. Other imaging tests may include CT and positron emission tomography, which also is called a PET scan.
-
Removing a sample of tissue for testing. A biopsy is a procedure to remove a sample of tissue for testing. It can be done with a needle before surgery or during surgery to remove the glioblastoma. The sample is sent to a lab for testing. Tests can tell whether the cells are cancerous and if they're glioblastoma cells.
Special tests of the cancer cells can give your health care team more information about your glioblastoma and your prognosis. The team uses this information to create a treatment plan.
Treatment
Glioblastoma treatment may begin with surgery. But surgery isn't always an option. For example, if the glioblastoma grows deeper into the brain, it might be too risky to remove all of the cancer. Other treatments, such as radiation therapy and chemotherapy, might be recommended as the first treatment.
Which treatments are best for you will depend on your particular situation. Your healthcare team considers the size of the glioblastoma and where it's located in the brain. Your treatment plan also depends on your health and your preferences.
Glioblastoma treatment options include:
Surgery to remove the glioblastoma
A brain surgeon, also known as a neurosurgeon, works to remove as much of the cancer as possible. Glioblastoma often grows into the healthy brain tissue, so it might not be possible to remove all of the cancer cells. Most people have other treatments after surgery to kill the cancer cells that are left.
Radiation therapy
Radiation therapy treats cancer with powerful energy beams. The energy can come from sources such as X-rays and protons. During radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to certain points in your brain.
Radiation therapy is usually recommended after surgery to kill any remaining cancer cells. It might be combined with chemotherapy. For people who can't have surgery, radiation therapy and chemotherapy may be the main treatment.
Chemotherapy
Chemotherapy treats cancer with strong medicines. A chemotherapy medicine taken as a pill is often used after surgery and during and after radiation therapy. Other types of chemotherapy given through a vein might be the treatment for glioblastoma that returns.
Sometimes thin, circular wafers containing chemotherapy medicine might be put in the brain during surgery. The wafers dissolve slowly, releasing the medicine to kill cancer cells.
Tumor treating fields therapy
Tumor treating fields therapy, also known as TTF, is a treatment that uses electrical energy to damage the glioblastoma cells. TTF makes it hard for the cells to multiply.
During this treatment, sticky pads are attached to the scalp. You might need to shave your head so that the pads can stick. Wires connect the pads to a portable device. The device generates an electrical field that damages the glioblastoma cells.
TTF works with chemotherapy. It might be suggested after radiation therapy.
Targeted therapy
Targeted therapy uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die.
Your glioblastoma cells may be tested to see if targeted therapy might help you. Targeted therapy is sometimes used after surgery if the glioblastoma can't be removed completely. Targeted therapy also may be used for glioblastoma that comes back after treatment.
Clinical trials
Clinical trials are studies of new treatments. These studies provide a chance to try the latest treatments. The risk of side effects might not be known. Ask your healthcare professional if you might be able to be in a clinical trial.
Treatments to control symptoms
If your glioblastoma is causing symptoms, you might need medicine to make you more comfortable. Which medicines you need depends on your situation. Options might include:
- Medicine to control seizures.
- Steroid medicines to reduce brain swelling.
- Medicine to help with headaches.
Palliative care
Palliative care is a special type of healthcare that helps someone with a serious illness feel better. If you have cancer, palliative care can help relieve pain and other symptoms. A healthcare team that may include doctors, nurses and other specially trained health professionals provides palliative care. The care team's goal is to improve quality of life for you and your family.
Palliative care specialists work with you, your family and your care team. They provide an extra layer of support while you have cancer treatment. You can have palliative care at the same time you're getting strong cancer treatments, such as surgery, chemotherapy or radiation therapy.
The use of palliative care with other medical treatments can help people with cancer feel better and live longer.
Alternative medicine
Alternative medicine therapies can't cure glioblastoma. But some integrative treatments can be combined with your healthcare team's care to help you cope with cancer treatment and side effects, such as distress.
People with cancer often feel distress. If you're distressed, you may have difficulty sleeping and find that you are constantly thinking about your cancer.
Discuss your feelings with your healthcare team. Specialists can help you come up with strategies for coping. For some people, medicines may help.
Integrative medicine treatments that may help you feel better include:
- Art therapy.
- Exercise.
- Massage therapy.
- Meditation.
- Music therapy.
- Relaxation exercises.
- Spirituality.
Talk with your healthcare team if you're interested in these treatment options.
Coping and support
With time, you'll find what helps you cope with the uncertainty and worry of a cancer diagnosis. Until then, you may find it helps to:
Learn enough about glioblastoma to make decisions about your care
Ask your healthcare team about your cancer, including your test results, treatment options and, if you like, your prognosis. As you learn more about glioblastoma, you may become more confident in making treatment decisions.
Keep friends and family close
Keeping your close relationships strong can help you deal with glioblastoma. Friends and family can provide the practical support you may need, such as helping take care of your home if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by having cancer.
Find someone to talk with
Find someone who is willing to listen to you talk about your hopes and worries. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
Ask your healthcare team about support groups in your area. Other sources of information include the National Cancer Institute and the American Cancer Society.
Preparing for an appointment
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you.
If your healthcare professional thinks you might have a brain tumor, such as glioblastoma, you may be referred to a specialist. Specialists who care for people with glioblastoma include:
- Doctors who specialize in brain nervous system diseases, called neurologists.
- Doctors who use medicine to treat cancer, called medical oncologists.
- Doctors who use radiation to treat cancer, called radiation oncologists.
- Doctors who specialize in brain and nervous system cancers, called neuro-oncologists.
- Surgeons who operate on the brain and nervous system, called neurosurgeons.
Because appointments can be brief, it's a good idea to be prepared. Here's some information to help you get ready.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down symptoms you have, including any that may not seem related to the reason for which you scheduled the appointment.
- Write down important personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements you're taking and the doses.
- Take a family member or friend along. Sometimes it can be very hard to remember all the information provided during an appointment. Someone who goes with you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
Your time with your healthcare team is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For glioblastoma, some basic questions to ask include:
- In what part of the brain is my cancer located?
- Has my cancer spread to other parts of my body?
- Will I need more tests?
- What are the treatment options?
- How much does each treatment increase my chances of a cure?
- What are the potential side effects of each treatment?
- How will each treatment affect my daily life?
- Is there one treatment option you believe is the best?
- What would you recommend to a friend or family member in my situation?
- Should I see a specialist?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
- What will determine whether I should plan for a follow-up visit?
Don't hesitate to ask other questions.
What to expect from your doctor
Be prepared to answer questions, such as:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?