Dizziness
Updated: 2024-11-02
Overview
Dizziness is a term that people use to describe a range of sensations, such as feeling faint, woozy, weak or wobbly. The sense that you or your surroundings are spinning or moving is more precisely termed vertigo.
Dizziness is one of the more common reasons adults see a healthcare professional. Frequent dizzy spells or constant dizziness can have serious effects on your life. But dizziness rarely means that you have a life-threatening condition.
Treatment of dizziness depends on the cause and your symptoms. Treatment often helps, but the symptoms may come back.
Symptoms
People who have bouts of dizziness may describe symptoms such as:
- A sense of motion or spinning, also called vertigo.
- Lightheadedness or feeling faint.
- A loss of balance or the sense of not feeling steady.
- A feeling of floating, wooziness or heavy-headedness.
These feelings may be triggered or made worse by walking, standing up or moving your head. Your dizziness may happen along with an upset stomach. Or your dizziness may be so sudden or severe that you need to sit or lie down. The bout may last seconds or days, and it may come back.
When to see a doctor
In general, see your healthcare professional if you have any repeated, sudden, severe, or long-lasting dizziness or vertigo with no clear cause.
Get emergency medical care if you have new, severe dizziness or vertigo along with any of the following:
- Pain such as a sudden, severe headache or chest pain.
- Rapid or irregular heartbeat.
- Loss of feeling or movement in the arms or legs, stumbling or trouble walking, or loss of feeling or weakness in the face.
- Trouble breathing.
- Fainting or seizures.
- Trouble with the eyes or ears, such as double vision or a sudden change in hearing.
- Confusion or slurred speech.
- Ongoing vomiting.
Causes
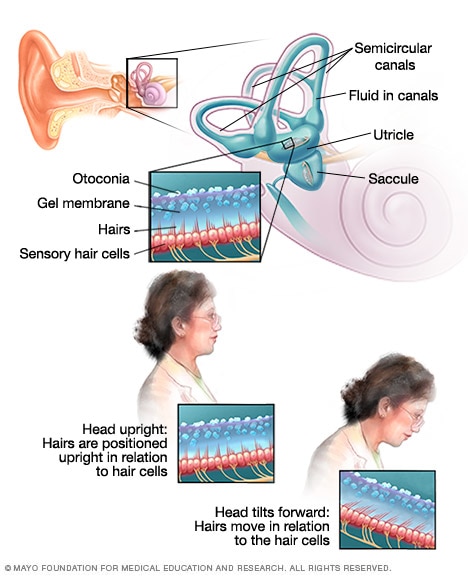
How the inner ear affects balance
Loop-shaped canals in the inner ear contain fluid and fine, hairlike sensors that help with keeping balance. At the base of the canals are the utricle and saccule, each containing a patch of sensory hair cells. Within these cells are tiny particles called otoconia that help monitor the position of the head in relation to gravity and linear motion, such as going up and down in an elevator or moving forward and backward in a car.
Dizziness has many possible causes. These include conditions that affect the inner ear, motion sickness and medicine side effects. Very rarely, dizziness may be caused by a condition such as poor circulation, infection or injury.
The way dizziness makes you feel and the things that trigger it for you provide clues about possible causes. How long the dizziness lasts and any other symptoms that you have also can help healthcare professionals pinpoint the cause.
Inner ear conditions that cause dizziness due to vertigo
Your sense of balance depends on the combined input from the various parts of your sensory system. These include your:
- Eyes, which help you figure out where your body is in space and how it's moving.
- Sensory nerves, which send messages to your brain about body movements and positions.
- Inner ear, which houses sensors that help detect gravity and back-and-forth motion.
Vertigo is the sense that your surroundings are spinning or moving. With inner ear conditions, your brain receives signals from the inner ear that don't match what your eyes and sensory nerves are receiving. Vertigo is what results as your brain works to sort out the confusion.
- Benign paroxysmal positional vertigo (BPPV). This condition causes an intense and brief sense that you're spinning or moving. These bouts are triggered by a rapid change in head movement. These changes in head movement can happen when you turn over in bed, sit up or get hit in the head. BPPV is the most common cause of vertigo.
- Viral infection. A viral infection called vestibular neuritis can cause intense, constant vertigo. It's an infection of the main nerve that leads from the inner ear to the brain, called the vestibular nerve. If you also have sudden hearing loss, you may have a condition called labyrinthitis. It can be caused by a virus, and it affects the nerve in the brain that controls balance and hearing.
- Migraine. People who get migraines may have bouts of vertigo or other types of dizziness even when they're not having bad headaches. Such vertigo bouts can last minutes to hours. They may be linked with headache as well as with being sensitive to light and noise.
- Meniere's disease. This rare disease involves the buildup of too much fluid in the inner ear. It causes sudden bouts of vertigo that can last for hours. It also can cause hearing loss that may come and go, ringing in the ear, and the feeling of a plugged ear.
Circulation problems that cause dizziness
You may feel dizzy, faint or off balance if too little blood reaches your brain. Causes include:
- Drop in blood pressure. A form of low blood pressure called orthostatic hypotension may make you briefly feel faint or dizzy. This type of low blood pressure happens after sitting up or standing too quickly.
- Poor blood flow. Conditions such as cardiomyopathy, heart attack, irregular heartbeat and transient ischemic attack could cause dizziness. Also, a drop in the total amount of blood flowing through the body may cause the brain or inner ear not to receive enough blood.
Other causes of dizziness
Dizziness may result from conditions or circumstances like these:
- Nervous system conditions. Some conditions that affect the brain, spinal cord or parts of the body controlled by nerves can lead to a loss of balance that becomes worse over time. These conditions include Parkinson's disease and multiple sclerosis.
- Medicines. Dizziness can be a side effect of certain medicines. These include anti-seizure medicines, antidepressants, sedatives and tranquilizers. Medicines that lower blood pressure may cause faintness if they lower blood pressure too much.
- Anxiety disorders. Certain types of anxiety may cause lightheadedness or a woozy feeling often referred to as dizziness. These include panic attacks and a fear of leaving home or being in large, open spaces. This fear is called agoraphobia.
- Anemia. There are several conditions that result in having too few healthy red blood cells, also called anemia. Other symptoms that may happen along with dizziness if you have anemia include fatigue, weakness and pale skin.
- Low blood sugar. Another name for this is hypoglycemia. This condition usually happens in people with diabetes who use insulin to help lower blood sugar. Dizziness may happen along with sweating and anxiety. If you have missed a meal and are hungry, that may cause unpleasant symptoms, but this is not considered hypoglycemia.
- Carbon monoxide poisoning. Symptoms of carbon monoxide poisoning are often described as flu-like. The symptoms include headache, dizziness, weakness, upset stomach, vomiting, chest pain and confusion.
- Overheating or not enough hydration. If you're active in hot weather or if you don't drink enough fluids, you may feel dizzy from overheating or from not being hydrated enough. The risk is even higher if you take certain heart medicines.
Risk factors
Factors that may raise your risk of getting dizzy include:
- Age. Older adults are more likely to have health conditions that cause dizziness, especially a sense of less balance. They're also more likely to take medicines that can cause dizziness.
- A past bout of dizziness. If you've had dizziness before, you're more likely to get dizzy in the future.
Complications
Dizziness can lead to other health concerns called complications. For instance, it can raise your risk of falling and hurting yourself. Getting dizzy while driving a car or running heavy machinery can make an accident more likely. You also may have long-term complications if you don't get treatment for a health condition that may be causing your dizziness.
Diagnosis
Diagnosis involves the steps your healthcare professional takes to find the cause of your dizziness or vertigo. You may need imaging tests such as an MRI or a CT scan right away if your healthcare professional thinks you might be having or may have had a stroke. You also may need one of these imaging tests if you are older or had a blow to the head.
Your healthcare professional asks you about your symptoms and the medicines you take. Then you'll likely have a physical exam. During this exam, your healthcare professional checks how you walk and maintain your balance. The major nerves of your central nervous system also are checked to make sure they're working.
You also may need a hearing test and balance tests, including:
- Eye movement testing. Your healthcare professional may watch the path of your eyes when you track a moving object. And you may be given an eye motion test in which water or air is placed in your ear canal.
- Head movement testing. If your vertigo may be caused by benign paroxysmal positional vertigo (BPPV), your healthcare professional may do a simple head movement test. It's called the Dix-Hallpike maneuver, and it can confirm that you have BPPV.
- Posturography. This test tells your healthcare professional which parts of the balance system you rely on the most and which parts may be giving you problems. You stand barefoot on a platform and try to keep your balance under various conditions.
- Rotary chair testing. During this test you sit in a computer-controlled chair that moves very slowly in a full circle. At faster speeds, it moves back and forth in a very small arc.
You also may be given blood tests to check for infection. You may need other tests to check your heart and blood vessel health too.
Treatment
Dizziness often gets better without treatment. The body usually adapts to whatever is causing the condition within a few weeks.
If you seek treatment, your treatment is based on the cause of your condition and your symptoms. Treatment may include medicines and balance exercises. Even if no cause is found or if your dizziness keeps happening, prescription medicines and other treatments may make your symptoms better.
Medications
- Water pills. If you have Meniere's disease, your healthcare professional may prescribe a water pill, also called a diuretic. This medicine along with a low-salt diet may help you have bouts of dizziness less often.
- Medicines that relieve dizziness and upset stomach. Your healthcare professional may prescribe medicines to provide fast relief from vertigo, dizziness and upset stomach. These medicines include prescription antihistamines and anticholinergics. Many of these medicines cause drowsiness.
- Anti-anxiety medications. Diazepam (Valium) and alprazolam (Xanax) are in a class of drugs called benzodiazepines. These can cause addiction. They also can cause drowsiness.
- Preventive medicine for migraine. Certain medicines can help prevent migraine attacks.
Therapy
- Head position movements. A technique called canalith repositioning or the Epley maneuver involves a series of head movements. The technique usually helps benign paroxysmal positional vertigo get better more quickly than simply waiting for dizziness to go away. It can be done by your healthcare professional, an audiologist or a physical therapist. It often works after one or two treatments. Before you get canalith repositioning, tell your healthcare professional if you have a neck or back condition, a detached retina, or a condition that affects blood vessels.
- Balance therapy. You may learn exercises to help make your balance system less sensitive to motion. This physical therapy technique is called vestibular rehabilitation. It is used for people with dizziness from inner ear conditions such as vestibular neuritis.
- Talk therapy. This involves talking with a psychologist, a psychiatrist or another mental healthcare professional. This type of therapy may help people whose dizziness is caused by anxiety.
Surgery or other procedures
- Injections. Your healthcare professional may inject your affected inner ear with the antibiotic gentamicin. This medicine stops the inner ear's balance function. Your other, healthy ear takes over that function.
- Removal of the inner ear sense organ. A treatment that's rarely used is called labyrinthectomy. A surgeon removes the parts of the ear causing vertigo. This causes complete hearing loss in that ear. The other ear takes over the balance function. This technique may be used if you have serious hearing loss and your dizziness hasn't gotten better after other treatments.
Lifestyle and home remedies
If you tend to have repeated bouts of dizziness, follow these tips:
- Be aware of the risk of losing your balance. This can lead to falls and serious injury. Walk with a cane for balance if needed. And try not to make fast or sudden movements.
- Fall-proof your home. Remove tripping hazards such as area rugs and exposed electrical cords. Use nonslip grip mats on your bath and shower floors. Use good lighting.
- Sit or lie down right away when you feel dizzy. Lie still with your eyes closed in a darkened room if you have a major bout of vertigo.
- Don't drive a car or run heavy machinery if you often become dizzy without warning.
- Limit use of caffeine, alcohol, salt and tobacco. Too much use of these substances can make your symptoms worse.
- Drink enough fluids, eat a healthy diet, get enough sleep and manage stress.
- If your dizziness comes with an upset stomach, try medicine called an antihistamine. Get the kind that's sold without a prescription. Examples include meclizine (Dramamine Less Drowsy) and dimenhydrinate (Dramamine). These might make you sleepy. But antihistamines that don't have this side effect aren't as effective.
If you know why you become dizzy, you can take steps such as these:
- If your dizziness is caused by a medicine, talk with your healthcare professional about lowering the dose or safely stopping the medicine.
- If your dizziness is caused by overheating or not being hydrated enough, rest in a cool place and drink water or a sports drink (Gatorade, Powerade, others).
Preparing for an appointment
Your main healthcare professional likely will be able to find and treat the cause of your dizziness. You may be referred to an ear, nose and throat doctor called otolaryngologist. Or you may see a doctor called a neurologist who treats conditions of the brain and nervous system.
Here's some information to help you get ready for your appointment.
What you can do
Take a family member or friend with you to the appointment if you can. Someone who goes with you can help you remember the information you get. Other things to do before the appointment include:
- Be aware of any restrictions before the appointment. Ask your healthcare professional's office if there's anything you need to do before your checkup. For instance, you may need to restrict your diet. If you need vestibular testing, your healthcare team gives you instructions about any medicines you shouldn't take the night before. You're also given information about what to eat on the day of testing.
- Be prepared to describe your dizziness in specific terms. When you have a bout of dizziness, do you feel like the room is spinning, or like you are spinning in the room? Do you feel like you might pass out? Your description of these symptoms is key to helping your healthcare professional find the cause.
- List any other health conditions or symptoms you have. Include any that may not seem related to your dizziness. For example, if you have felt depressed or anxious recently, this is important information for your healthcare team.
- List key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements that you take. Include medicines and supplements that you bought with or without prescriptions.
- List questions to ask your healthcare professional.
For dizziness, some basic questions to ask your healthcare professional include:
- What's the most likely cause of my symptoms?
- Are there any other possible causes for my symptoms?
- What tests do you recommend?
- Is this problem likely short term or long lasting?
- Is it possible my symptoms will go away without treatment?
- What treatment options might help?
- Do I need to follow any restrictions? For example, is it safe for me to drive?
- Should I see a specialist?
- Is there a generic version of the medicine you're prescribing?
- Do you have any brochures or other printed material that I can take home with me? What websites do you recommend?
What to expect from your doctor
Your healthcare professional likely will ask you questions such as:
- Can you describe what you felt the first time you became dizzy?
- Is your dizziness ongoing, or does it happen in bouts or spells? If your dizziness happens in bouts, how long do these bouts last?
- How often do your dizziness bouts happen? When do they seem to happen, and what triggers them?
- Does your dizziness cause the room to spin or produce a sense of motion?
- When you feel dizzy, do you also feel faint or lightheaded? Do you lose your balance?
- Do your symptoms happen along with a ringing or fullness in your ears, trouble hearing, or blurred vision?
- Is your dizziness made worse by moving your head?
- What medicines, vitamins or supplements are you taking?
What you can do in the meantime
If you tend to feel lightheaded when you stand up, take your time making changes in posture. If you have had bouts of dizziness while driving, have someone else drive you in the weeks before your healthcare checkup. For instance, you could ask a relative or friend to drive you as needed. Or you could use a rideshare service or public transportation.
If your dizziness causes you to feel like you might fall, take steps to lower your risk. Keep your home well lighted and free of hazards that might cause you to trip. Remove area rugs and clear away exposed electrical cords. Place furniture where you're not likely to bump into it. And use nonslip grip mats in the bathtub and on shower floors.