Abdominal aortic aneurysm
Updated: 2023-04-25
Overview
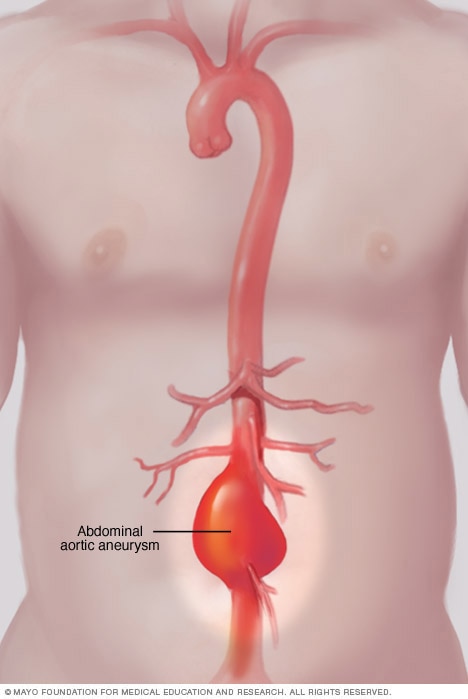
Abdominal aortic aneurysm
An abdominal aortic aneurysm occurs when a lower part of the body's main artery, called the aorta, becomes weakened and bulges.
An abdominal aortic aneurysm is an enlarged area in the lower part of the body's main artery, called the aorta. The aorta runs from the heart through the center of the chest and belly area, called the abdomen.
The aorta is the largest blood vessel in the body. An abdominal aortic aneurysm that ruptures can cause life-threatening bleeding.
Treatment depends on the size of the aneurysm and how fast it's growing. Treatment varies from regular health checkups and imaging tests to emergency surgery.
Symptoms
Abdominal aortic aneurysms often grow slowly without noticeable symptoms. This makes them difficult to detect. Some aneurysms never rupture. Many start small and stay small. Others grow larger over time, sometimes quickly.
If you have a growing abdominal aortic aneurysm, you might notice:
- Deep, constant pain in the belly area or side of the belly.
- Back pain.
- A pulse near the bellybutton.
When to see a doctor
If you have pain, especially if pain is sudden and severe, seek medical help right away.
Causes
Aneurysms can develop anywhere along the aorta. Most aortic aneurysms occur in the part of the aorta that's in the belly area, called the abdomen. Several things can lead to the development of an abdominal aortic aneurysm, including:
- Hardening of the arteries, called atherosclerosis. Atherosclerosis occurs when fat and other substances build up on the lining of a blood vessel.
- High blood pressure. High blood pressure can damage and weaken the aorta's walls.
- Blood vessel diseases. These are diseases that cause blood vessels to become inflamed.
- Infection in the aorta. Rarely, infection by certain bacteria or fungi might cause an abdominal aortic aneurysm.
- Trauma. For example, being injured in a car accident can cause an abdominal aortic aneurysm.
Risk factors
Abdominal aortic aneurysm risk factors include:
- Tobacco use. Smoking is the strongest risk factor for aortic aneurysms. Smoking can weaken the walls of blood vessels, including the aorta. This raises the risk of aortic aneurysm and aneurysm rupture. The longer and more you use tobacco, the greater the chances are of developing an aortic aneurysm. Men ages 65 to 75 who are current or former smokers should have a one-time ultrasound to screen for an abdominal aortic aneurysm.
- Age. Abdominal aortic aneurysms occur most often in people age 65 and older.
- Being male. Men develop abdominal aortic aneurysms much more often than women do.
- Being white. People who are white are at higher risk of abdominal aortic aneurysms.
- Family history. Having a family history of abdominal aortic aneurysms increases the risk of having the condition.
- Other aneurysms. Having an aneurysm in the aorta in the chest (thoracic aortic aneurysm) or in another large blood vessel, such as the artery behind the knee, might increase the risk of an abdominal aortic aneurysm.
If you're at risk of an aortic aneurysm, medicines may be given to lower your blood pressure and relieve stress on weakened arteries.
Complications
Complications of abdominal aortic aneurysms include:
- Tears in one or more of the layers of the wall of the aorta, called an aortic dissection.
- Rupture of the aneurysm.
A rupture can cause life-threatening internal bleeding. In general, the larger the aneurysm and the faster it grows, the greater the risk of rupture.
Symptoms that an aortic aneurysm has ruptured can include:
- Sudden, intense and persistent belly or back pain, which may feel like ripping or tearing.
- Low blood pressure.
- Fast pulse.
Aortic aneurysms also increase the risk of developing blood clots in the area. If a blood clot breaks loose from the inside wall of an aneurysm, it can block a blood vessel elsewhere in the body. Symptoms of a blocked blood vessel may include pain or reduced blood flow to the legs, toes, kidneys or belly area.
Prevention
To prevent an abdominal aortic aneurysm or to keep one from worsening, do the following:
- Don't smoke or use tobacco products. If you smoke or chew tobacco, quit. Also avoid secondhand smoke. If you need help quitting, talk to your health care provider about strategies that may help.
- Eat a healthy diet. Choose a variety of fruits and vegetables, whole grains, chicken, fish, and low-fat dairy products. Avoid saturated and trans fats and limit salt.
- Keep your blood pressure and cholesterol under control. If your care provider prescribed medicines, take them as instructed.
- Get regular exercise. Try to get at least 150 minutes a week of moderate aerobic activity. If you haven't been active, start slowly and build up. Talk to your health care provider about what kinds of activities are right for you.
Diagnosis
Abdominal aortic aneurysms are often found when a physical exam or imaging test is done for another reason.
To diagnose an abdominal aortic aneurysm, the health care provider examines you and reviews your medical and family history.
Tests to diagnose an abdominal aortic aneurysm include:
- Abdominal ultrasound. This is the most common test to diagnose abdominal aortic aneurysms. Sound waves are used to show how blood flows through the structures in the belly area, including the aorta.
- Abdominal CT scan. This test uses X-rays to create cross-sectional images of the structures inside the belly area. It can create clear images of the aorta. This test also can detect the size and shape of an aneurysm.
- Abdominal MRI. This imaging test uses a magnetic field and computer-generated radio waves to create detailed images of the structures inside the belly area.
During some CT and MRI scans, a liquid called contrast may be given through a vein to make the blood vessels show up more clearly on the images.
Screening for abdominal aortic aneurysm
Being male and smoking significantly increase the risk of abdominal aortic aneurysm. Screening recommendations vary, but in general:
- Men ages 65 to 75 who have ever smoked cigarettes should have a one-time screening using abdominal ultrasound.
- For men ages 65 to 75 who have never smoked, the need for an abdominal ultrasound is based on other risk factors, such as a family history of aneurysm.
Women who have never smoked generally don't need to be screened for abdominal aortic aneurysm. There isn't enough evidence to say whether women ages 65 to 75 with a history of smoking or a family history of abdominal aortic aneurysm benefit from screening. Ask your health care provider if screening is right for you.
Treatment
The goal of abdominal aortic aneurysm treatment is to prevent an aneurysm from rupturing. Treatment may involve:
- Frequent health checkups and imaging, called medical monitoring or watchful waiting.
- Surgery.
Which treatment you have depends on the size of the abdominal aortic aneurysm and how fast it's growing.
Frequent health checkups
If the abdominal aortic aneurysm is small and isn't causing symptoms, you may only need frequent health checkups and imaging tests to see if the aneurysm is growing.
Typically, a person with a small, symptom-free abdominal aortic aneurysm needs an ultrasound at least six months after diagnosis. Abdominal ultrasounds also should be done at regular follow-up appointments.
During the regular checkups, a health care provider also checks for conditions, such as high blood pressure, that could make an aneurysm worse.
Surgery and other procedures
Surgery to repair an abdominal aortic aneurysm is generally recommended if the aneurysm is 1.9 to 2.2 inches (4.8 to 5.6 centimeters) or larger, or if it's growing quickly.
Repair surgery also may be recommended if you have symptoms such as stomach pain or have a leaking, tender or painful aneurysm.
The type of surgery done depends on:
- The size and location of the aneurysm.
- Your age.
- Your overall health.
Abdominal aortic aneurysm treatment options may include:
-
Endovascular repair. This treatment is most often used to repair an abdominal aortic aneurysm. A surgeon inserts a thin, flexible tube, called a catheter, through an artery in the groin area and guides it to the aorta. A metal mesh tube on the end of the catheter is placed at the site of the aneurysm. The mesh tube, called a graft, expands, and strengthens the weakened area of the aorta. This helps prevent rupture of the aneurysm.
Endovascular surgery isn't an option for everyone with an abdominal aortic aneurysm. You and your health care team should discuss the best repair option for you. Regular imaging tests are done after this treatment to make sure the blood vessel isn't leaking.
- Open surgery. This is major surgery. A surgeon removes the damaged part of the aorta and replaces it with a graft, which is sewn into place. Full recovery may take a month or more.
Long-term survival rates are similar for both endovascular surgery and open surgery.
Lifestyle and home remedies
Your health care provider may tell you to avoid heavy lifting and vigorous physical activity. These activities may cause extreme increases in blood pressure, which can worsen an aneurysm.
Emotional stress also can raise blood pressure. Try to avoid conflict and stressful situations. If you're feeling stressed or anxious, let your care provider know. Together you can come up with the best treatment plan.
Preparing for an appointment
Make an appointment with your health care provider if you are concerned about your risk of an abdominal aortic aneurysm. If you're having severe pain, seek emergency medical help.
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as avoid food or drinks for a period of time.
Make a list of:
- Your symptoms, including any that may seem unrelated to an abdominal aortic aneurysm, and when they began.
- Important personal information, including a family history of heart disease or aneurysms.
- All medicines, vitamins or other supplements you take. Include the dosages.
- Questions to ask your health care provider.
For an abdominal aortic aneurysm, questions to ask your health care provider include:
- What's the most likely cause of my symptoms?
- What tests will I need?
- What treatments are available? Which do you think would be the best treatment for me?
- Do I need regular screenings, and if so, how often?
- I have other health conditions. How can I best manage these conditions together?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your health care provider is likely to ask you questions, including:
- Do your symptoms come and go, or do you always feel them?
- How severe are your symptoms?
- Does anything improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Have you ever smoked?